Tonsillitis, a common inflammatory condition of the tonsils, can be quite unpleasant. This summary explores various management approaches, empowering you to understand and navigate your treatment options.
Understanding the Culprit:
Tonsillitis can be caused by:
- Bacteria: Most commonly Group A Streptococcus (GAS), responsible for “strep throat.”
- Viruses: Viruses like Epstein-Barr (EBV) or adenovirus cause viral tonsillitis.
- Other Factors: Allergies, irritants, and rarely, fungal infections can contribute.
Differentiating the Enemy:
Symptoms can overlap, but some subtle differences exist:
- Bacterial: Sudden onset, high fever, intense sore throat, white or yellow pus on tonsils, swollen lymph nodes.
- Viral: Gradual onset, lower fever, milder sore throat, cough, runny nose, headache.
Diagnosis and Investigation:
- Medical history and physical examination: Discussing symptoms and checking for fever, swollen tonsils, and pus.
- Rapid strep test: Quick test to detect GAS (not definitive for other causes).
- Throat swab culture: Confirms bacterial infection if rapid test is negative or inconclusive.
- Blood tests: Rarely needed but may assess other causes like mono.
Treatment Strategies:
The approach depends on the cause and severity:
Bacterial Tonsillitis:
- Antibiotics: Penicillin-based medication is the mainstay, taken for 10 days to eradicate the bacteria.
- Pain relievers: Over-the-counter medications like ibuprofen or acetaminophen help manage fever and discomfort.
- Rest and hydration: Crucial for recovery and preventing complications.
Viral Tonsillitis:
- Supportive care: Rest, fluids, pain relievers, and throat lozenges are the cornerstones.
- Antibiotics are ineffective: Do not take unless a secondary bacterial infection develops.
Additional Options:
- Gargling with warm salt water: Soothes sore throat and promotes healing.
- Humidifier: Moist air eases nasal congestion and throat discomfort.
- Ice packs: Applied to the neck can relieve swollen lymph nodes.
Surgery (Tonsillectomy):
- Reserved for recurrent tonsillitis (5-7 episodes/year), sleep apnea caused by enlarged tonsils, or other complications.
- Minimally invasive techniques are often used for faster recovery.
Remember:
- Early diagnosis and treatment are crucial, especially for bacterial tonsillitis to prevent complications like rheumatic fever.
- Complete the antibiotic course even if symptoms improve to eradicate the infection.
- Consult your doctor if symptoms worsen, don’t improve within 48 hours, or you suspect complications.
- Preventive measures like frequent handwashing and avoiding close contact with sick individuals can help reduce the risk of tonsillitis.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
SORE THROAT
In-Depth Management of a Sore Throat: Finding Relief and Fast
Sore throats, a common ailment plaguing people of all ages, can range from mild irritations to debilitating discomfort. This comprehensive guide dives into understanding and managing sore throats for a swift return to vocal ease.
Understanding the Source:
Sore throats can originate from various causes, each requiring different approaches:
- Viruses: Most frequent culprits, responsible for the “common cold” and its sore throat symptom.
- Bacteria: Strep throat, caused by Group A Streptococcus, presents with sudden onset, high fever, and intense pain.
- Allergies: Dust, pollen, and pet dander can trigger allergy-induced sore throats.
- Irritants: Smoke, dry air, and chemical fumes can irritate throat tissues, causing discomfort.
- Other factors: Acid reflux, dehydration, and even dental issues can contribute to sore throats.
Pinpointing the Culprit:
Accurate diagnosis guides effective treatment. Consider:
- Symptom evaluation: Sudden onset, fever, swollen glands, pus on tonsils suggest bacterial infection.
- Physical examination: Doctor checks throat, ears, and lymph nodes for signs of inflammation.
- Rapid strep test: Quick in-office test to detect strep throat.
- Throat swab culture: In inconclusive cases, confirms bacterial infection.
Treatment Tailored to the Cause:
Viral Sore Throat:
- Supportive care: Rest, fluids, pain relievers like ibuprofen or acetaminophen, and throat lozenges ease discomfort.
- No antibiotics: They won’t fight viruses, and overuse can lead to antibiotic resistance.
Bacterial Sore Throat (Strep Throat):
- Antibiotics: Penicillin-based medications eradicate the bacteria and prevent complications like rheumatic fever.
- Complete the full course: Even if symptoms improve, finishing the antibiotics ensures complete bacterial elimination.
- Pain relievers: Manage fever and discomfort while antibiotics work.
Other Treatments:
- Gargling with warm salt water: Soothes the throat and reduces inflammation.
- Humidifier: Adds moisture to the air, easing irritation and promoting healing.
- Ice packs: Applied to the neck can relieve swollen lymph nodes.
When to Seek Help:
- Severe or persistent sore throat (lasting more than 7 days)
- High fever (above 101°F for adults, 103°F for children)
- Difficulty swallowing or breathing
- Swollen glands
- Symptoms of dehydration
- Blood in saliva
Prevention Tips:
- Frequent handwashing
- Avoiding close contact with sick individuals
- Managing allergies
- Using a humidifier when air is dry
- Staying hydrated
- Getting enough sleep
Remember:
- Early diagnosis and treatment are crucial for a speedy recovery and to prevent complications.
- If you suspect strep throat, seek medical attention promptly.
- Don’t hesitate to discuss your concerns and treatment options with your healthcare provider.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
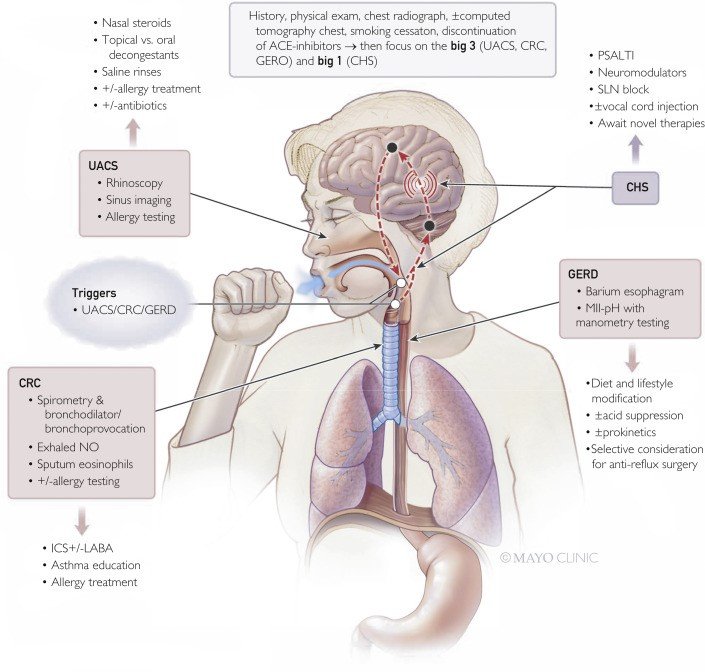
CHRONIC COUGH
Delving Deep into Chronic Cough Management: A Comprehensive Guide
Chronic cough, defined as a cough lasting beyond eight weeks, can significantly impact daily life. Effective management requires a tailored approach based on the underlying cause. This detailed summary unravels the various causes, diagnostic steps, and treatment options for chronic cough, empowering you with crucial knowledge.
Understanding the Culprits:
Chronic cough can stem from various sources, categorized into:
- Respiratory: Asthma, postnasal drip, chronic bronchitis, bronchiectasis, interstitial lung disease, tuberculosis.
- Non-respiratory: Gastroesophageal reflux disease (GERD), medications (ACE inhibitors), smoking, environmental irritants.
- Psychological: Habit cough, psychogenic cough.
Unveiling the Mystery:
Diagnosing the root cause begins with:
- Detailed medical history: Discussing your cough characteristics, duration, associated symptoms, and potential triggers.
- Physical examination: Checking for signs of respiratory issues or GERD.
- Chest X-ray and lung function tests: Evaluating lung health and airflow.
- Additional tests: Depending on suspicion, tests like bronchoscopy (visualizing airways), allergy testing, or esophageal pH monitoring (checking for GERD) may be recommended.
Tailoring the Treatment:
Once the cause is identified, specific treatments are employed:
- Respiratory causes: Bronchodilators, inhaled corticosteroids, antibiotics (for infections), cough suppressants (use cautiously due to potential side effects).
- Non-respiratory causes: GERD medications, smoking cessation, allergen avoidance, medication adjustments.
- Psychological causes: Relaxation techniques, therapy.
Additional Strategies:
- Hydration: Drinking plenty of fluids helps thin mucus and ease coughing.
- Humidifier: Adds moisture to the air, soothing irritated airways.
- Saltwater gargling: Can alleviate postnasal drip and throat irritation.
- Honey (for adults only): May provide mild cough relief, but consult your doctor first.
Important Considerations:
- Over-the-counter cough suppressants: Use cautiously due to potential side effects and ineffectiveness for chronic cough.
- Antibiotics: Only effective for bacterial infections, not recommended for other causes.
- Smoking cessation: Crucial for overall lung health and cough improvement.
- Seeking professional help: Early diagnosis and appropriate treatment are key to managing chronic cough effectively.
Remember:
- Chronic cough management is a personalized journey based on the underlying cause.
- Open communication with your doctor is crucial throughout the process.
- There is no “one-size-fits-all” solution, and patience is essential for finding the most effective approach.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
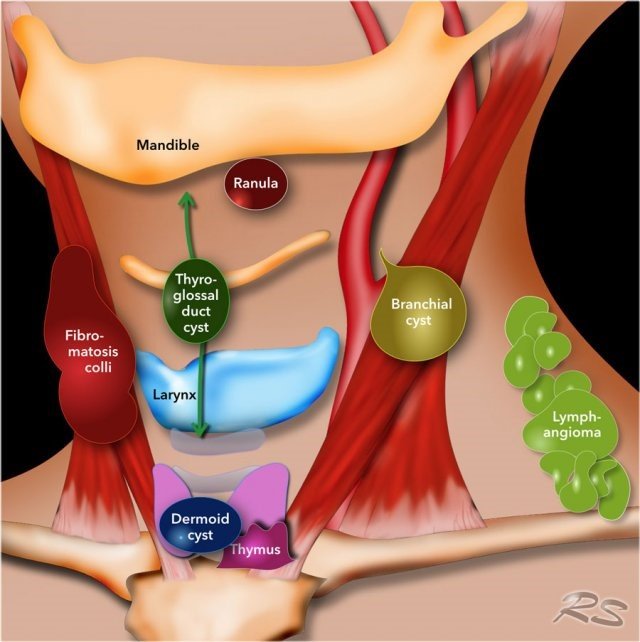
NECK LUMPS
Managing Neck Masses: A Comprehensive Guide
Neck masses, often presenting as lumps or bumps, can be concerning, but understanding their origins and management options can bring peace of mind. This detailed summary delves into the various aspects of managing neck masses.
Understanding the Culprit:
Neck masses can arise from various sources, impacting diagnosis and treatment:
- Lymphadenopathy: Enlarged lymph nodes, often due to:
- Benign. Infection, inflammation, or immune system response.
- Malignant: Metastatic cancer deposit in the neck nodes
- Thyroid nodules: Growths in the thyroid gland, generally benign but some requiring attention.
- Salivary gland masses: Non-cancerous or cancerous lumps in the salivary glands.
- Branchial cleft cysts: Remnants of embryonic development, usually benign but sometimes needing removal.
- Lipoma: Fatty tumors, typically harmless but potentially requiring cosmetic removal.
- Other: Vascular malformations, sebaceous cysts, and malignant tumors are less common possibilities.
Seeking Evaluation:
Early diagnosis is crucial. Consult your doctor if you experience:
- A new, persistent neck mass (lasting over 2 weeks)
- Rapidly growing mass
- Painful or tender mass
- Difficulty swallowing or breathing
- Weight loss, fever, or night sweats
Diagnosis and Investigation:
- Medical history and physical examination: Discussing symptoms and assessing the mass’ characteristics.
- Fine-needle aspiration biopsy (FNAB): Thin needle extracts cells for microscopic examination, often the first step.
- Imaging tests: Ultrasound, CT scan, or MRI to assess mass size, location, and internal features.
- Blood tests: Check for thyroid function, infection markers, or other underlying conditions.
Treatment Options:
The approach depends on the underlying cause and characteristics of the mass:
Benign Lymph Nodes:
- Observation: In some cases, monitoring is sufficient, especially for self-resolving infections.
- Antibiotics: For bacterial infections.
- Surgical removal: For persistent or concerning enlarged nodes.
Suspicious / Malignant Lymph Nodes:
- Referral: After appropriate investigation, we refer the patient to H&N specialist
- Investigations:
- Histology: Fine Needle aspiration (FNAc), Core biopsy, Open biopsy
- Radiology: USS, CT scan, MRI, PET scan
- Treatment: Treatment of underlying malignancy (Cancer Unit)
Thyroid Nodules:
- Monitoring: For small, benign nodules with normal thyroid function.
- Fine-needle aspiration: Further confirms benignancy or guides treatment.
- Thyroid medication: For nodules affecting hormone production.
- Surgery: For large, suspicious, or symptomatic nodules.
Other Masses:
- Observation: For some benign masses like lipomas.
- Surgical removal: The most common approach for most other types of masses.
- Medical treatments: Specific medications or radiation therapy for certain cancers.
Remember:
- Early diagnosis and proper management are crucial to ensure optimal outcomes.
- Not all neck masses are cancerous, but seeking professional evaluation is essential.
- Open communication with your doctor regarding your concerns and treatment options is key.
- Support groups and patient resources can be helpful during the diagnosis and treatment journey.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
SWALLOWING PROBLEMS
Managing Swallowing Problems: A Comprehensive Guide
Swallowing difficulties, also known as dysphagia, can significantly impact your quality of life. This detailed guide explores the causes, diagnosis, and various management options to help you regain control of your swallowing function.
Understanding the Culprit:
Dysphagia can arise from various factors affecting different stages of the swallow:
- Oral phase: Problems with chewing, holding food in the mouth, or initiating the swallow reflex.
- Pharyngeal phase: Difficulty moving food from the mouth to the esophagus due to weak muscles, incoordination, or nerve impairment.
- Esophageal phase: Obstructions in the esophagus from narrowing (strictures), weak muscles, or abnormal contractions (achalasia).
Common Causes:
- Neurological conditions: Stroke, Parkinson’s disease, dementia, head injury, nerve disorders.
- Structural issues: Tumors, esophageal strictures, Zenker’s diverticulum.
- Muscle weakness: Myopathies, aging-related changes.
- Gastrointestinal disorders: Gastroesophageal reflux disease (GERD), achalasia.
- Other: Medications, dental problems, psychological factors.
Identifying the Problem:
- Detailed history: Discussing symptoms, swallowing difficulties, and underlying medical conditions.
- Physical examination: Assessing oral cavity, muscle strength, and sensation.
- Swallowing evaluation: Videofluoroscopy (VFSS) is the gold standard, using X-rays to visualize swallowing motions.
- Other tests: Endoscopy, manometry, barium swallow may be used in specific cases.
Treatment Tailored to Your Needs:
The chosen approach depends on the cause and severity of dysphagia:
Dietary modifications: Changing food and drink consistencies (e.g., thicker liquids, pureed foods) and textures to make swallowing safer and easier. Swallow therapy: Exercises and techniques to improve muscle strength, coordination, and sensory awareness during swallowing. Postural techniques: Specific head and body positions during swallowing to optimize food passage. Medications: To manage GERD, relax esophageal muscles, or address underlying conditions. Surgical interventions: for structural issues or severe cases refractory to other approaches.
Additional Tools:
- Thickeners: Powders to adjust beverage consistency.
- Feeding tubes: Temporary or permanent tubes delivering nutrition directly to the stomach or intestine in severe cases.
- Support groups: Connect with others facing similar challenges.
Remember:
- Early diagnosis and intervention are crucial to prevent complications like malnutrition, dehydration, and aspiration pneumonia.
- Treatment success depends on individual factors and adherence to the management plan.
- Open communication with your healthcare team is essential to determine the best approach for you.
- Don’t hesitate to seek support and resources to improve your quality of life.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
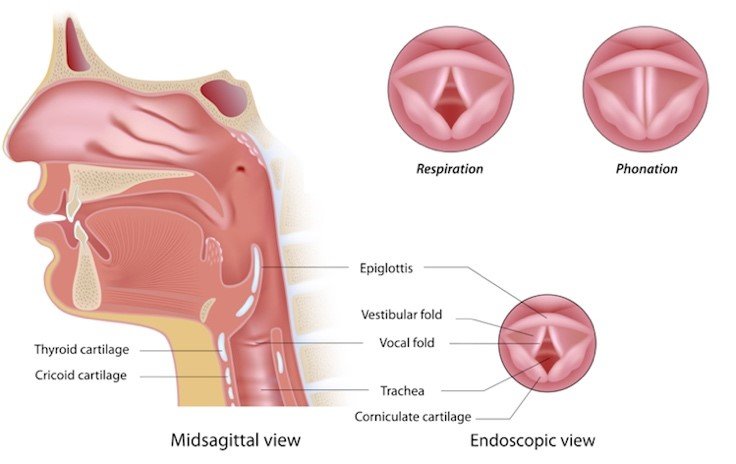
VOICE CHANGES
Navigating Vocal Changes: A Comprehensive Guide to Management
Changes in voice quality, pitch, or volume can be unsettling. This detailed summary explores the diverse causes, diagnosis, and management options to help you restore your voice to its rightful melody.
Understanding the Culprit:
Voice changes can stem from various factors, impacting the way sound is produced:
- Structural abnormalities: Vocal nodules, polyps, cysts, or vocal fold paralysis can obstruct or alter vocal cord vibration.
- Neurological conditions: Parkinson’s disease, stroke, or nerve damage can disrupt muscle control and coordination.
- Infections: Laryngitis, tonsillitis, and respiratory infections can inflame the larynx and vocal cords.
- Overuse or misuse: Excessive vocal strain, yelling, or improper singing techniques can damage vocal cords.
- Aging: Weakening muscles and reduced lubrication can lead to hoarseness or breathiness.
- Other factors: Allergies, acid reflux, hormonal changes, and certain medications can affect voice quality.
Identifying the Cause:
- Detailed history: Discussing your voice changes, duration, associated symptoms, and medical history.
- Physical examination: Examining the larynx and vocal cords using a mirror or stroboscopy (visualizing vocal fold vibration).
- Laryngoscopy: Direct visualization of the larynx through a flexible scope in some cases.
- Imaging tests: CT scan or MRI (rarely) to assess anatomy and rule out structural abnormalities.
Treatment Tailored to the Cause:
- Vocal hygiene: Resting your voice, avoiding irritants, staying hydrated, and practicing good speaking habits.
- Voice therapy: Exercises and techniques to improve vocal cord function, reduce strain, and optimize your voice.
- Medical treatment: Antibiotics for infections, medications for allergies or reflux, and hormone therapy for hormonal imbalances.
- Surgery: Removal of nodules, polyps, or scar tissue in severe cases.
- Augmentation: Injections or implants to plump vocal cords in specific situations.
Additional Recommendations:
- Speech-language pathologist (SLP) consultation: Provides specialized assessment and voice therapy.
- Lifestyle modifications: Managing stress, getting enough sleep, and quitting smoking can promote vocal health.
- Support groups: Connecting with others facing similar challenges can offer emotional support and resources.
Remember:
- Early diagnosis and intervention are crucial to prevent further damage and ensure optimal outcomes.
- The appropriate treatment depends on the underlying cause and individual needs.
- Working closely with your healthcare team and following the management plan is key to restoring your voice.
- Be patient and persistent, as voice rehabilitation often takes time and dedication.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
THYROID MASSES
Navigating the Tides: A Comprehensive Guide to Managing Thyroid Masses
Thyroid masses, lumps or bumps in the thyroid gland, can be concerning, but navigating their management with knowledge and a proactive approach empowers you to make informed decisions. This detailed summary explores the intricacies of thyroid masses, from causes and diagnosis to various management options.
Understanding the Landscape:
Thyroid masses encompass a spectrum of possibilities:
- Benign nodules: The most common type, often harmless, but requiring monitoring.
- Thyroid cysts: Fluid-filled sacs, usually benign but sometimes needing drainage.
- Follicular adenomas: Non-cancerous growths, but with a small risk of becoming cancerous.
- Papillary thyroid carcinoma: The most common thyroid cancer, often highly treatable.
- Other less common thyroid cancers: Medullary, anaplastic, and Hürthle cell carcinomas.
Pinpointing the Culprit:
Early diagnosis is crucial. Seek medical attention if you experience:
- A new, persistent neck mass (lasting over 2 weeks)
- Rapidly growing mass
- Painful or tender mass
- Difficulty swallowing or breathing
- Hoarseness
- Changes in thyroid function (hyperthyroidism or hypothyroidism)
Charting the Course:
Diagnosis starts with:
- Detailed history and physical examination: Discussing symptoms and palpating the thyroid gland.
- Ultrasound: Assesses mass size, location, and characteristics.
- Fine-needle aspiration cytology (FNAc): Thin needle extracts cells for microscopic examination, often the first step.
- Blood tests: Thyroid function tests and sometimes cancer markers.
Management Options:
The approach depends on the mass type, size, and potential for cancer:
Benign Nodules:
- Monitoring: Regular checkups and ultrasounds to track changes.
- FNAc: Repeated if the mass grows or becomes suspicious.
- Surgery: For large, bothersome, or suspicious nodules.
Thyroid Cysts:
- Aspiration: Draining the fluid and monitoring.
- Surgery: If large, recurring, or suspicious.
Follicular Adenomas:
- FNAc: To confirm benignity or guide further management.
- Surgery: Often the preferred option, especially if large or concerning.
- Radioactive iodine (RAI) therapy: To destroy remaining thyroid tissue after surgery and suppress TSH levels.
Papillary Thyroid Carcinoma:
- Surgery: Primary treatment, usually removing the entire or part of the thyroid gland.
- RAI therapy: Destroys any remaining thyroid tissue and helps detect and treat potential spread.
- Thyroid medication: Suppresses TSH levels and prevents recurrence.
Other Thyroid Cancers:
- More complex treatment plans involving surgery, RAI therapy, chemotherapy, and targeted therapy, depending on the specific cancer type and stage.
Remember:
- Early diagnosis and proper management increase the chances of a successful outcome.
- Not all thyroid masses are cancerous, but seeking professional evaluation is crucial.
- Open communication with your doctor regarding your concerns and treatment options is key.
- Support groups and patient resources can be invaluable sources of information and understanding.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.