GROMMETS INSERTION
Diving Deep into Grommet Insertion: A Comprehensive Guide
Grommet insertion, also known as tympanostomy tube placement, is a common surgical procedure aimed at improving ventilation and drainage in the middle ear. This detailed summary unveils the procedure’s purpose, preparation, steps, benefits, risks, and recovery to offer a complete understanding.
Understanding the Cause:
Chronic ear infections, otitis media with effusion (OME), and glue ear often cause fluid build-up behind the eardrum, impacting hearing and increasing the risk of further infections. Grommets provide a temporary drainage pathway, alleviating these issues.
Preparing for the Big Day:
- Pre-operative assessment: Your doctor will discuss your medical history, perform a physical examination, and may request hearing tests to evaluate the need for grommets.
- Anaesthesia: General anaesthesia is typically used for children, while local anaesthesia with sedation may be used for older individuals.
- Medications: Stop taking certain medications like blood thinners as advised by your doctor.
- Fasting: Follow specific instructions regarding food and drink restrictions before the surgery.
The Step-by-Step Journey:
- Anaesthesia administration: You will be comfortably put under anaesthesia.
- Microscopic examination: The surgeon uses a microscope for magnified visualization of the eardrum.
- Incision: A tiny incision is made in the eardrum.
- Grommet insertion: A small, plastic tube (grommet) is carefully inserted through the incision into the middle ear.
- Closure: The incision may be left open to heal naturally or closed with tiny stitches that dissolve over time.
- Recovery: You will be monitored in a recovery room before being discharged, depending on the type of anaesthesia used.
Benefits:
- Improved hearing: By draining excess fluid, grommets help restore hearing and prevent hearing loss associated with persistent fluid build-up.
- Reduced infections: By promoting ventilation and preventing fluid stagnation, grommets can significantly reduce the frequency and severity of ear infections.
- Pain relief: Drainage of fluid often alleviates discomfort and pressure associated with ear infections.
Risks and Complications:
- Minor bleeding: Bleeding from the incision site is usually minimal and temporary.
- Infection: Though rare, ear infections or inflammation around the grommet can occur.
- Grommet extrusion: The grommet may fall out prematurely before the natural healing process.
- Tympanic membrane perforation: In rare cases, the eardrum may not close completely after the grommet falls out.
Recovery and Beyond:
- Ear drops: You may be prescribed ear drops to prevent infection and promote healing.
- Water precautions: Avoid getting water in your ears for a specific period, as advised by your doctor.
- Follow-up visits: Regular checkups are crucial to monitor healing, grommet status, and hearing improvement.
Additional Information:
- The procedure typically takes 15-30 minutes.
- Grommets usually stay in place for 6-18 months, eventually falling out naturally.
- The decision to insert grommets depends on individual factors and severity of the underlying condition.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
MYRINGOPLASTY
Detailed Summary of Myringoplasty: Eardrum Repair Surgery
What is Myringoplasty?
Myringoplasty is a surgical procedure designed to repair a perforation (hole) in the eardrum (tympanic membrane). This perforation can be caused by various factors such as:
- Ear infections: A common cause, especially in children.
- Trauma: Injury from a cotton swab, foreign objects, or sudden pressure changes (e.g., explosion, airplane descent).
- Loud noises: In rare cases, very loud noises can rupture the eardrum.
Why is Myringoplasty Performed?
A perforated eardrum can lead to several problems, including:
- Hearing loss: The hole disrupts sound wave transmission, causing conductive hearing loss.
- Ear infections: The perforation creates an open pathway for bacteria and water to enter the middle ear, increasing the risk of infections.
- Balance problems: In some cases, the middle ear connects to the inner ear, which plays a role in balance. A perforated eardrum can affect this connection and cause balance issues (less common).
Myringoplasty aims to:
- Close the hole in the eardrum: This restores the eardrum’s integrity and prevents further complications.
- Improve hearing: By repairing the eardrum, the procedure can significantly improve conductive hearing loss.
- Reduce the risk of infections: Sealing the perforation helps prevent bacteria and water from entering the middle ear.
Who is a Candidate for Myringoplasty?
Myringoplasty may be recommended for individuals who have:
- A persistent hole: If the perforation hasn’t healed on its own within a timeframe (usually 6-12 months).
- Hearing loss: Conductive hearing loss due to a perforated eardrum.
- Recurrent ear infections: Frequent infections related to the perforation.
- Vertigo or balance problems: Less common, but sometimes associated with the perforation.
The Myringoplasty Procedure (Outpatient Surgery):
Preparation:
- Pre-operative assessment: A thorough medical history review and physical examination are conducted. The ENT surgeon will use an otoscope (lighted instrument) to examine the eardrum, assess the size, location, and cause of the perforation. Hearing tests may also be performed.
- Anaesthesia: The procedure can be performed under various anaesthesia options depending on the patient’s age, medical condition, and surgeon’s preference:
- General anaesthesia
- Local anaesthesia with sedation
- Local anaesthesia alone
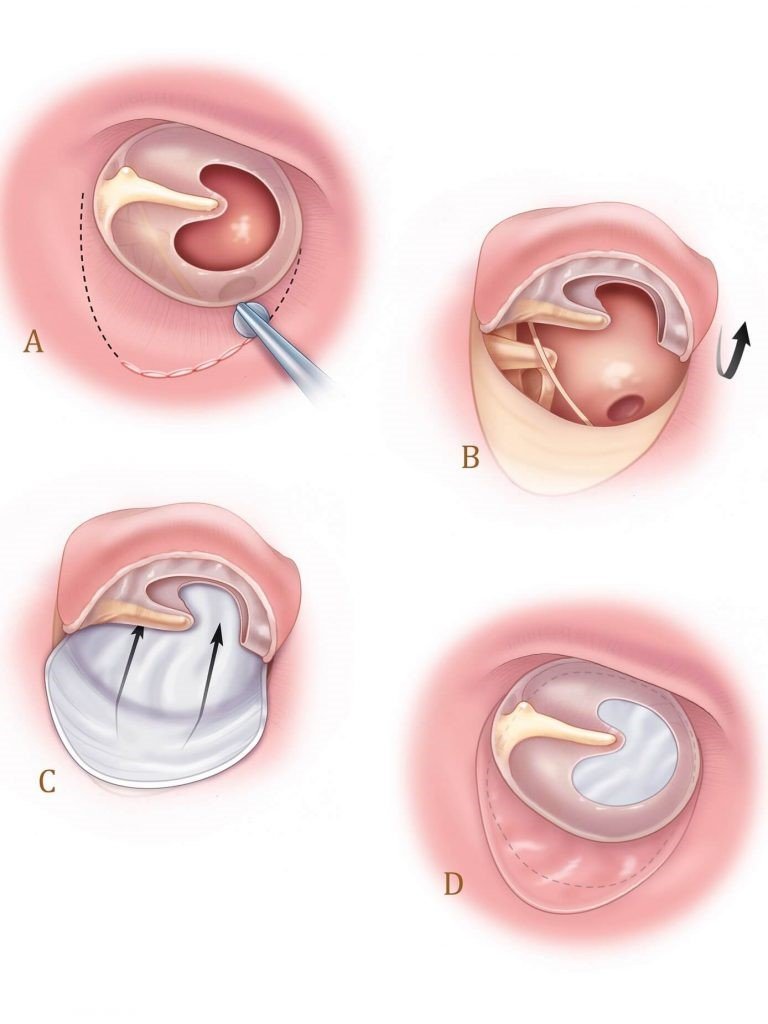
The Procedure:
- Access: The surgeon needs to access the middle ear space. There are two main approaches:
- Postauricular approach: An incision is made behind the ear.
- Transcanal approach: An incision is made within the ear canal itself.
- Graft preparation: A patch material (graft) is needed to close the perforation. The type of graft can vary:
- Temporal fascia: Tissue from the underlying temporal muscle behind the ear (most common).
- Tragal cartilage: Cartilage from the tragus, a small bump in front of the ear canal.
- Synthetic materials: In some cases, synthetic materials may be used.
- Eardrum repair: The surgeon carefully positions the graft over the perforation and secures it using:
- Stitches
- Tissue adhesives
- Closure: The incision, either behind the ear or in the ear canal, is then closed with stitches or other appropriate methods.
Recovery from Myringoplasty:
Recovery from myringoplasty is usually smooth. Packing materials may be placed in the ear canal for a short period to support healing. Patients may experience some mild discomfort or earache for a few days, manageable with pain medication.
Post-operative Care:
- Ear care: Following the doctor’s instructions regarding ear care is crucial. This may include:
- Avoiding water exposure (swimming, bathing) for a certain period.
- Using earplugs in specific situations (e.g., showering).
- Keeping the ears clean and dry.
- Hearing: Hearing improvement can be noticeable within a few weeks or months after the procedure as the eardrum heals.
- Follow-up appointments: Regular follow-up appointments with the ENT surgeon are essential to monitor the healing process and check for any complications.
Benefits of Myringoplasty:
- Improved hearing: Repairing the eardrum can significantly improve conductive hearing loss.
- Reduced risk of infections: Sealing the perforation helps prevent bacteria and water from entering the middle ear.
- Prevention of further complications: Myringoplasty can prevent long-term issues like chronic ear infections or permanent
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
TYMPANOPLASTY
Detailed Summary of Tympanoplasty: Eardrum Reconstruction Surgery
Tympanoplasty is a surgical procedure designed to reconstruct the tympanic membrane (eardrum) and, in some cases, repair or rebuild associated structures within the middle ear. It offers a more comprehensive solution compared to myringoplasty, which focuses solely on repairing a simple perforation.
Why is Tympanoplasty Performed?
Tympanoplasty addresses a wider range of middle ear issues, including:
- Large or Complex Perforations: When a hole in the eardrum is extensive, involves multiple areas, or has ragged edges, myringoplasty may not be suitable. Tympanoplasty allows for a more complex reconstruction using various techniques and materials.
- Chronic Otitis Media (COM): Persistent inflammation or infection in the middle ear can benefit from tympanoplasty. The procedure removes diseased tissue and restores proper middle ear function.
- Ossicular Dysfunction: The tiny bones (ossicles) in the middle ear transmit sound vibrations. Tympanoplasty can address damage or dislocation of these bones, improving hearing.
- Cholesteatoma: This growth of abnormal skin cells in the middle ear can be removed and the surrounding structures reconstructed with tympanoplasty.
Types of Tympanoplasty:
The specific type of tympanoplasty is chosen based on the extent and nature of the damage:
- Myringoplasty: As discussed earlier, this is considered a type of tympanoplasty that focuses solely on repairing a perforation in the eardrum.
- Tympanoplasty Type I: Repairs a perforation without involving the ossicles.
- Tympanoplasty Type II: Repairs a perforation and addresses ossicular problems like dislocation or erosion. Techniques may involve repositioning the ossicles or using prosthetics to replace damaged bones.
- Tympanoplasty Type III (Type IIIa & IIIb): This involves the most extensive reconstruction. It includes removing diseased tissue, repairing the eardrum, and potentially rebuilding the ossicular chain or wall of the middle ear.
The Tympanoplasty Procedure (Outpatient or Inpatient Surgery):
The details of the procedure depend on the type of tympanoplasty and the complexity of the reconstruction. Here’s a general breakdown:
Preparation:
- Pre-operative assessment: A thorough medical history review and physical examination are conducted. The ENT surgeon uses an otoscope (lighted instrument) to examine the eardrum and assess the damage. Imaging tests like CT scans may be used for detailed evaluation. Hearing tests are also performed.
- Anaesthesia: The procedure is typically performed under general anaesthesia, especially for children or complex cases. Local anaesthesia with sedation may be an option for simpler procedures in adults.
The Procedure:
- Access: The surgeon needs to access the middle ear space. Approaches can vary depending on the type of tympanoplasty:
- Postauricular approach: An incision is made behind the ear for most extensive procedures.
- Transcanal approach: An incision is made within the ear canal itself for simpler procedures.
- Middle Ear Exploration: The surgeon examines the middle ear structures, removes any diseased tissue (e.g., in cholesteatoma cases), and assesses the extent of damage to the eardrum and ossicles.
- Eardrum Reconstruction: Similar to myringoplasty, a graft material (often temporal fascia) is used to repair the perforation and reshape the eardrum.
- Ossicle Repair/Reconstruction (if needed): Depending on the type of tympanoplasty, procedures may involve:
- Repositioning dislocated ossicles
- Using prosthetics to replace damaged ossicles
- Utilizing ossicular grafts from other sources (e.g., cartilage, bone)
- Closure: The incision is then closed with stitches or other appropriate methods. Packing materials may be placed in the ear canal for a short period to support healing.
Recovery from Tympanoplasty:
Recovery from tympanoplasty can vary depending on the complexity of the procedure:
- Hospital stays: You may stay in the hospital overnight for observation, especially for complex procedures.
- Discomfort: You may experience some mild discomfort or earache for a few days, manageable with pain medication.
- Ear care: Following the doctor’s instructions regarding ear care is crucial. This may include:
- Avoiding water exposure (swimming, bathing) for a certain period.
- Using earplugs in specific situations (e.g., showering).
- Keeping the ears clean and dry.
- Hearing: Hearing improvement can take weeks or months as the eardrum heals and any ossicular reconstruction settles.
Benefits of Tympanoplasty:
Tympanoplasty offers a range of potential benefits for individuals experiencing problems due to a damaged eardrum:
- Improved Hearing: By repairing the eardrum, tympanoplasty restores proper sound transmission to the middle ear, leading to improved hearing ability. This can benefit people who experience muffled hearing, difficulty understanding speech, or increased sensitivity to loud noises.
- Reduced Risk of Infection: A large or persistent perforation creates an opening for bacteria and water to enter the middle ear, leading to recurrent infections. Tympanoplasty closes this opening, significantly reducing the risk of future infections.
- Prevention of Further Damage: Over time, a damaged eardrum can deteriorate further. Tympanoplasty prevents this progression and protects the delicate structures of the middle ear.
- Pain Relief: In some cases, a damaged eardrum can cause discomfort or pain. Tympanoplasty can alleviate this discomfort by restoring a normal eardrum structure.
- Improved Quality of Life: Overall, successful tympanoplasty can significantly improve a person’s quality of life. With better hearing and reduced risk of infections, individuals can experience a renewed sense of well-being and participation in various aspects of life.
It’s important to note that the success rate of tympanoplasty and the degree of hearing improvement vary depending on the individual case and the specific procedure performed. However, for many individuals, tympanoplasty offers a chance to regain lost hearing function and prevent further complications.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
OSSICULOPLASTY
Deep Dive into Ossiculoplasty: Restoring the Sound Transmission Chain
Ossiculoplasty is a microsurgical procedure designed to reconstruct or replace the tiny bones (ossicles) in the middle ear. These bones, the malleus, incus, and stapes, play a crucial role in transmitting sound vibrations from the eardrum to the inner ear, where they are converted into electrical signals for the brain to interpret as sound.
Why Choose Ossiculoplasty?
There are several reasons why a doctor might recommend ossiculoplasty:
- Conductive Hearing Loss: Damage or disruption to the ossicular chain can lead to conductive hearing loss, where sound waves are not transmitted efficiently to the inner ear. Ossiculoplasty aims to restore proper sound conduction and improve hearing.
- Ossicle Erosion: Chronic otitis media (COM) or cholesteatoma can erode or destroy these delicate bones, necessitating reconstruction.
- Ossicle Dislocation: Trauma or congenital malformations can cause the ossicles to become dislodged, affecting their ability to vibrate and transmit sound. Ossiculoplasty can reposition the bones for improved function.
- Congenital Abnormalities: Some individuals are born with missing or malformed ossicles, leading to hearing problems from birth. Ossiculoplasty can offer a solution.
Types of Ossiculoplasty:
The specific type of ossiculoplasty depends on the extent and nature of the damage to the ossicular chain:
- Partial Ossiculoplasty: This involves replacing one or two of the ossicles with prosthetics made of various materials like titanium or Teflon.
- Total Ossiculoplasty: This involves replacing the entire ossicular chain with a single prosthetic device called a columella.
- Incus Replacement: The incus, the middle ossicle, is the most commonly affected bone. Ossiculoplasty can replace it with a prosthesis.
- Stapes Surgery: In some cases, the stapes itself might require procedures like stapedectomy (removal) or stapedotomy (placement of a small prosthesis) to improve sound transmission.
The Ossiculoplasty Procedure (Outpatient or Inpatient Surgery):
The details of the procedure depend on the type of ossiculoplasty and the complexity of the reconstruction. Here’s a breakdown of the general steps:
Pre-Operative Assessment:
- Medical History & Physical Examination: Your doctor will review your medical history and perform a physical examination, focusing on the ears.
- Otoscopy: The ENT surgeon uses a lighted instrument (otoscope) to examine the middle ear and assess the damage to the ossicles.
- Imaging Tests: CT scans may be used for detailed evaluation of the middle ear structures, especially in complex cases.
- Hearing Tests: Baseline hearing tests are conducted to establish a reference point for monitoring improvement after surgery.
- Anaesthesia: The procedure is typically performed under general anaesthesia, especially for children or complex cases. Local anaesthesia with sedation may be an option for simpler procedures in adults.
Surgical Steps:
- Access to the Middle Ear: The surgeon needs to access the middle ear space. Approaches can vary depending on the complexity:
-
- Postauricular approach: An incision is made behind the ear for most extensive procedures.
- Transcanal approach: An incision is made within the ear canal itself for simpler procedures.
- Middle Ear Exploration: The surgeon examines the middle ear structures, removes any diseased tissue (e.g., in cholesteatoma cases), and assesses the extent of damage to the ossicles.
- Ossicle Repair/Reconstruction: Depending on the type of ossiculoplasty, procedures may involve:
-
- Removing damaged ossicles
- Replacing ossicles with prosthetics
- Repositioning dislocated ossicles
- Utilizing ossicular grafts from other sources (e.g., cartilage, bone)
- Closure: The incision is then closed with stitches or other appropriate methods. Packing materials may be placed in the ear canal for a short period to support healing.
Recovery from Ossiculoplasty:
Recovery from ossiculoplasty can vary depending on the complexity of the procedure:
- Hospital Stay: You may stay in the hospital overnight for observation, especially for complex procedures.
- Discomfort: You may experience some mild discomfort or earache for a few days, manageable with pain medication.
- Ear Care: Following the doctor’s instructions regarding ear care is crucial. This may include:
- Avoiding water exposure (swimming, bathing) for a certain period.
- Using earplugs in specific situations (e.g., showering).
- Keeping the ears clean and dry.
- Hearing: Hearing improvement can take weeks or months as the eardrum heals and any ossicular reconstruction settles
Benefits of Ossiculoplasty:
Ossiculoplasty offers a range of potential benefits for individuals experiencing conductive hearing loss:
- Improved Hearing: The primary benefit of ossiculoplasty is the potential for significant improvement in hearing ability. By repairing or replacing damaged ossicles, the procedure restores the proper transmission of sound vibrations, leading to better perception of speech, music, and other sounds.
- Reduced Hearing Loss: Ossiculoplasty addresses conductive hearing loss caused by:
-
- Dislocated ossicles
- Erosion of ossicles due to chronic otitis media or cholesteatoma
- Congenital malformations of the ossicles
By correcting these issues, the procedure effectively reduces the degree of hearing loss experienced by the patient.
- Enhanced Communication and Social Interaction: Improved hearing translates to better communication and social interaction. Individuals who regain hearing after ossiculoplasty can participate more actively in conversations, enjoy listening to music and media, and reconnect with loved ones.
- Increased Confidence and Self-Esteem: Hearing loss can lead to feelings of isolation and reduced self-esteem. Successful ossiculoplasty can significantly improve a person’s confidence by allowing them to engage more fully in social and professional settings.
- Improved Quality of Life: Overall, ossiculoplasty can significantly enhance a person’s quality of life. With better hearing, individuals can experience a renewed sense of connection, independence, and participation in various aspects of life.
- Additional Potential Benefits:
-
- In some cases, ossiculoplasty may also address tinnitus (ringing in the ears) associated with conductive hearing loss.
- By removing diseased tissue during the procedure (e.g., in cholesteatoma cases), ossiculoplasty can help prevent further complications in the middle ear.
It’s important to note that the success rate of ossiculoplasty and the degree of hearing improvement vary depending on the individual case and the specific procedure performed. However, for many individuals, ossiculoplasty offers a chance to regain lost hearing and enjoy the associated benefits for a better quality of life.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
MASTOIDECTOMY
Mastoidectomy: Exploring the Procedure to Remove Diseased Mastoid Cells
A mastoidectomy is a surgical procedure that removes diseased cells from the air-filled spaces in the mastoid bone, located just behind the ear. These spaces, called mastoid air cells, can become infected or develop abnormal growths, necessitating intervention.
Why Perform a Mastoidectomy?
There are several reasons why a doctor might recommend a mastoidectomy:
- Chronic Mastoiditis: This is a persistent infection within the mastoid bone, often stemming from a previous middle ear infection (otitis media) that has spread. Symptoms include persistent ear drainage, pain, swelling, and potentially facial weakness.
- Cholesteatoma: This is an abnormal growth of skin-like tissue in the middle ear that can erode surrounding bone, including the mastoid. Mastoidectomy is necessary for complete removal of cholesteatoma and prevention of recurrence.
- Facial Nerve Complications: In severe cases of mastoiditis or cholesteatoma, the facial nerve, responsible for facial movement, can become involved. Mastoidectomy can help prevent or address damage to this nerve.
- Cochlear Implant Placement: In some cases, a mastoidectomy creates access to the middle ear for cochlear implant placement, a device that helps individuals with severe hearing loss perceive sound.
Types of Mastoidectomy:
The specific type of mastoidectomy depends on the extent and nature of the disease:
- Simple Mastoidectomy (Antrostomy): This is a less extensive procedure that removes diseased tissue from the mastoid antrum, the largest air cell cavity.
- Radical Mastoidectomy: This is a more comprehensive procedure that removes all mastoid air cells along with diseased tissue in the middle ear cavity. It aims for complete eradication of cholesteatoma or chronic infection.
- Modified Radical Mastoidectomy: This falls between simple and radical, removing most but not all mastoid air cells while preserving healthy middle ear structures.
The Mastoidectomy Procedure (Inpatient or Outpatient Surgery):
The details of the procedure depend on the type of mastoidectomy being performed. Here’s a general breakdown:
Pre-Operative Assessment:
- Medical History & Physical Examination: Your doctor will review your medical history and perform a physical examination, focusing on the ear and surrounding area.
- Imaging Tests: CT scans are often used to evaluate the extent of disease in the mastoid bone and middle ear.
- Hearing Tests: Baseline hearing tests may be conducted to establish a reference point for monitoring after surgery (not always necessary).
- Anaesthesia: The procedure is typically performed under general anaesthesia, especially for children or complex cases. Local anaesthesia with sedation may be an option for simpler procedures in adults.
Surgical Steps:
- Incision: The surgeon makes an incision behind the ear to access the mastoid bone.
- Bone Removal: Using drills and other instruments, the surgeon removes diseased bone and tissue from the mastoid air cells. In some cases, the middle ear cavity may also be accessed for further exploration and removal of diseased tissue.
- Facial Nerve Identification: During the procedure, the surgeon meticulously identifies and protects the facial nerve, which runs near the mastoid bone. 4. Closure: Once the diseased tissue is removed, the surgeon closes the incision with stitches or other appropriate methods. Packing materials may be placed in the ear canal for a short period to support healing.
Recovery from Mastoidectomy:
Recovery from a mastoidectomy can vary depending on the complexity of the procedure:
- Hospital Stay: You may stay in the hospital overnight for observation, especially for complex procedures.
- Discomfort: You may experience some pain, swelling, and bruising behind the ear for a few days. Pain medication can help manage discomfort.
- Ear Care: Following the doctor’s instructions regarding ear care is crucial. This may include:
- Avoiding water exposure (swimming, bathing) for a certain period.
- Using earplugs in specific situations (e.g., showering).
- Keeping the ears clean and dry.
- Hearing: In some cases, hearing may initially worsen after surgery, but it can improve over time as healing progresses.
- Facial Nerve Complications: While rare, there’s a small risk of facial nerve weakness or paralysis after surgery. This risk increases with more extensive procedures.
Benefits of Mastoidectomy:
Mastoidectomy offers several potential benefits for individuals experiencing complications in the mastoid bone and middle ear:
- Eradication of Infection: By removing infected tissue, mastoidectomy stops the spread of infection and prevents serious complications like meningitis or brain abscess. This significantly improves overall health and well-being.
- Removal of Cholesteatoma: Mastoidectomy provides the most effective way to remove cholesteatoma completely. This abnormal growth can erode surrounding bone and damage delicate structures. Removing it prevents further destruction and reduces the risk of recurrence.
- Improved Hearing: In some cases, mastoidectomy can improve hearing, especially when chronic infection or cholesteatoma has affected the ossicular chain (tiny bones) responsible for sound transmission. By removing diseased tissue and potentially reconstructing the ossicles, hearing can be restored or preserved.
- Reduced Pain and Discomfort: Persistent ear pain and discomfort can be a significant symptom of mastoiditis or cholesteatoma. Mastoidectomy removes the source of this pain, leading to significant improvement in quality of life.
- Prevention of Facial Nerve Complications: In severe cases of mastoiditis or cholesteatoma, the facial nerve can become involved, leading to weakness or paralysis. Mastoidectomy can help prevent this complication or address it in its early stages.
- Potential for Cochlear Implant Placement: In some situations, a mastoidectomy can create the necessary access to the middle ear for cochlear implant placement. This device helps individuals with severe hearing loss perceive sound and improve communication abilities.
Additional Considerations:
- While hearing improvement can occur, it’s not the primary goal of mastoidectomy. The main focus is removing diseased tissue and preventing complications.
- The success rate of mastoidectomy and the degree of hearing improvement vary depending on the individual case and the specific procedure performed.
- Mastoidectomy can be a complex surgery with potential risks, such as facial nerve weakness or injury. However, experienced surgeons strive to minimize these risks.
Overall, mastoidectomy offers a valuable solution for individuals experiencing mastoiditis, cholesteatoma, and other complications in the mastoid bone and middle ear. By removing diseased tissue and preventing further damage, it can significantly improve a person’s health, hearing, and quality of life.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
OTOPLASTY
Otoplasty: Reshaping the Ears for Enhanced Appearance and Confidence
Otoplasty is a cosmetic surgical procedure designed to correct or improve the shape, position, or size of the outer ear (pinna). It addresses a variety of aesthetic concerns, boosting self-esteem and confidence for individuals who feel self-conscious about their ears.
Who Can Benefit from Otoplasty?
Otoplasty is a suitable option for individuals experiencing:
- Protruding Ears: This is the most common reason for otoplasty. Ears that extend more than 2 centimetres from the side of the head or have an angle greater than 35 degrees are considered prominent.
- Lop Ears: The upper cartilage of the ear folds inward, creating a folded or crumpled appearance.
- Uneven Ears: The ears may be different sizes or shapes, causing asymmetry.
- Ear Defects: Birth defects or injuries may have caused ear malformations that otoplasty can address.
Otoplasty Techniques:
The specific technique used in otoplasty depends on the desired correction:
- Suture Techniques (Mustarde Technique): This is a common approach for prominent ears. Sutures are placed behind the ear cartilage to reshape and reposition it closer to the head. This technique creates a more natural fold in the antihelical fold (curved ridge) of the ear.
- Cartilage Scoring: In some cases, scoring (making small cuts) on the back of the ear cartilage weakens it, allowing for easier moulding into the desired shape. This technique is often combined with suturing.
- Conchal Cartilage Resection: If the bowl-shaped portion of the ear (concha) is excessively deep, otoplasty may involve removing a small portion of cartilage to create a more balanced appearance.
- Otoplasty for Lop Ears: This may involve a combination of scoring, suturing, and removal of a small wedge of cartilage to reshape the upper cartilage and create a more defined antihelical fold.
The Otoplasty Procedure (Typically Outpatient Surgery):
The details of the procedure depend on the complexity of the correction:
Pre-Operative Assessment:
- Consultation: You discuss your concerns and desired outcomes with a plastic surgeon. They will examine your ears, assess your medical history, and determine the most suitable technique.
- Imaging: In some cases, photographic documentation or 3D imaging may be used for planning purposes.
- Anaesthesia: Otoplasty is typically performed under local anaesthesia with sedation for adults and general anaesthesia for children.
Surgical Steps:
- Incision: Depending on the technique, the surgeon makes a discreet incision behind the ear or within the natural folds of the ear cartilage.
- Cartilage Reshaping: The surgeon reshapes the ear cartilage using scoring, suturing, or cartilage removal techniques as needed.
- Redraping Skin: The skin is redraped over the reshaped cartilage to create a smooth, natural appearance.
- Closure: The incision is closed with stitches or other appropriate methods. Bandages or dressings may be applied to the ears for support and protection.
Recovery from Otoplasty:
Recovery from otoplasty can vary depending on the complexity of the procedure:
- Discomfort: You may experience mild swelling, bruising, and discomfort for a few days after surgery. Pain medication can help manage discomfort.
- Bandages: You may need to wear a headband or dressing for a short period to support the ears during healing.
- Activity Restrictions: Strenuous activity and lifting heavy objects may be restricted for a few weeks to prevent complications.
- Follow-up Appointments: You will have regular follow-up appointments with your surgeon to monitor healing and ensure proper results.
Benefits of Otoplasty:
Otoplasty offers a range of potential benefits for individuals:
- Improved Appearance: Otoplasty can significantly improve the aesthetics of the ears, leading to a more balanced and proportional facial profile.
- Increased Confidence and Self-Esteem: Feeling self-conscious about prominent or misshapen ears can affect social interactions and self-esteem. Otoplasty can alleviate these concerns and boost confidence.
- Psychological Benefits: For individuals who have experienced teasing or bullying due to their ear shape, otoplasty can offer a sense of empowerment and improved self-image.
- Improved Quality of Life: Overall, successful otoplasty can significantly enhance a person’s quality of life by reducing self-consciousness and promoting a more positive self-perception.
Additional Considerations:
- Benefits for Children: Otoplasty can be performed on children as young as 6-7 years old, when the ears have reached nearly their full size. This can help prevent them from experiencing teasing or bullying during their formative years.
- Permanent Results: Otoplasty is typically a permanent procedure, offering long-lasting benefits for the individual.
- Individualized Approach: The specific benefits of otoplasty will vary depending on the person’s unique situation and desired outcomes.
It’s important to remember that otoplasty is an elective cosmetic surgery.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.