A blocked nose, medically known as nasal congestion, can be a constant source of discomfort and disrupt your daily life. This detailed summary delves into the various causes, diagnosis, and effective management strategies to help you breathe easy again.
Understanding the Culprit:
Several factors can lead to a blocked nose:
- Infections: The common cold, flu, and sinusitis are frequent culprits, causing inflammation and mucus production.
- Allergies: Exposure to allergens like pollen, dust mites, or pet dander triggers an immune response leading to congestion.
- Vasomotor rhinitis: Changes in temperature or humidity can irritate the nasal lining, causing swelling and congestion.
- Structural abnormalities: Deviated septum, nasal polyps, or enlarged adenoids in children can obstruct airflow.
- Environmental irritants: Smoke, dust, and strong odors can irritate the nasal passages and cause congestion.
- Medications: Certain medications, including decongestants if used excessively, can cause rebound congestion.
Identifying the Cause:
Accurate diagnosis helps determine the most effective treatment approach. Consider:
- Detailed history: Discussing the duration, severity, and associated symptoms like fever, facial pain, discharge, or allergy triggers.
- Physical examination: Examining the nose and throat for signs of inflammation, polyps, or structural issues.
- Allergy testing: Skin prick tests or blood tests can identify potential allergens.
- Imaging tests: X-rays or CT scans might be needed in specific cases to rule out structural problems.
Tailoring Treatment to the Cause:
The approach depends on the identified cause:
Infections:
- Over-the-counter (OTC) decongestants: Short-term relief for nasal congestion (avoid using these for more than 3-5 days due to rebound congestion).
- Saline nasal spray or irrigation: Moistens and thins mucus, aiding natural clearance.
- Rest and fluids: Promotes recovery and helps thin mucus.
Allergies:
- Antihistamines: H1-antihistamines block the release of allergy-causing chemicals.
- Nasal corticosteroids: Reduce inflammation and congestion in the long term.
- Allergy immunotherapy: Desensitizes the body to the allergen over time.
Vasomotor rhinitis:
- Saline nasal spray or irrigation: Moisturizes the nasal lining and reduces irritation.
- Nasal corticosteroids: Can be helpful for long-term management.
- Nasal antimuscarinics: Reduces nasal discharge
- Avoiding triggers: Limiting exposure to temperature changes or humidity extremes.
Structural abnormalities:
- Surgery: May be necessary to correct a deviated septum, remove polyps, or address enlarged adenoids.
Environmental irritants:
- Avoiding triggers: Wearing a mask outdoors, using air purifiers, and managing dust and smoke exposure.
Other Considerations:
- Humidifier: Adding moisture to the air can loosen mucus and ease congestion.
- Warm compresses: Applying warm compresses to the face can offer temporary relief.
- Elevating your head while sleeping: Helps promote drainage and reduce congestion.
- Managing stress: Stress can worsen congestion, so relaxation techniques can be beneficial.
Remember:
- Early diagnosis and management are crucial to prevent complications like sinusitis or ear infections.
- Different causes require different approaches, and individual factors influence treatment decisions.
- Open communication with your healthcare team regarding your concerns and treatment options is key.
- By understanding the diverse causes and available management strategies, you can breathe easier and reclaim a more comfortable life.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
NASAL CONGESTION
Clearing the Path: A Comprehensive Guide to Managing Nasal Congestion
Nasal congestion, that stuffy sensation in your nose, can range from a minor annoyance to a significantly disruptive force in your daily life. This detailed summary delves into the various causes, diagnosis, and effective management strategies to help you breathe freely and comfortably again.
Understanding the Culprit:
Several factors can lead to a blocked nose:
- Infections: Common culprits include the common cold, flu, and sinusitis, causing inflammation and increased mucus production.
- Allergies: Exposure to airborne allergens like pollen, dust mites, or pet dander triggers an immune response leading to congestion.
- Vasomotor rhinitis: Changes in temperature or humidity can irritate the nasal lining, causing swelling and congestion.
- Structural abnormalities: Deviated septum, nasal polyps, or enlarged adenoids (in children) can obstruct airflow.
- Environmental irritants: Smoke, dust, and strong odors can irritate the nasal passages and cause congestion.
- Medications: Certain medications, including decongestants if used excessively, can cause rebound congestion.
- Hormonal changes: Pregnancy and menstrual cycles can contribute to temporary congestion.
Identifying the Cause:
Accurate diagnosis helps determine the most effective treatment approach. Consider:
- Detailed history: Discussing the duration, severity, and associated symptoms like fever, facial pain, discharge, or allergy triggers.
- Physical examination: Examining the nose and throat for signs of inflammation, polyps, or structural issues.
- Allergy testing: Skin prick tests or blood tests can identify potential allergens.
- Imaging tests: X-rays or CT scans might be needed in specific cases to rule out structural problems.
Tailoring Treatment to the Cause:
The approach depends on the identified cause:
Infections:
- Over-the-counter (OTC) decongestants: Short-term relief for nasal congestion (use carefully and avoid exceeding 3-5 days due to rebound congestion).
- Saline nasal spray or irrigation: Moistens and thins mucus, aiding natural clearance.
- Rest and fluids: Promotes recovery and helps thin mucus.
Allergies:
- Antihistamines: H1-antihistamines block the release of allergy-causing chemicals.
- Nasal corticosteroids: Reduce inflammation and congestion in the long term.
- Allergy immunotherapy: Desensitizes the body to the allergen over time.
Vasomotor rhinitis:
- Saline nasal spray or irrigation: Moisturizes the nasal lining and reduces irritation.
- Nasal corticosteroids: Can be helpful for long-term management.
- Nasal antimuscarinics: Reduces nasal discharge
- Avoiding triggers: Limiting exposure to temperature changes or humidity extremes.
Structural abnormalities:
- Surgery: May be necessary to correct a deviated septum, remove polyps, or address enlarged adenoids.
Environmental irritants:
- Avoiding triggers: Wearing a mask outdoors, using air purifiers, and managing dust and smoke exposure.
Other Considerations:
- Humidifier: Adding moisture to the air can loosen mucus and ease congestion.
- Warm compresses: Applying warm compresses to the face can offer temporary relief.
- Elevating your head while sleeping: Helps promote drainage and reduce congestion.
- Managing stress: Stress can worsen congestion, so relaxation techniques can be beneficial.
- Nasal decongestant strips: Can provide temporary relief, but avoid overuse.
Remember:
- Early diagnosis and management are crucial to prevent complications like sinusitis or ear infections.
- Different causes require different approaches, and individual factors influence treatment decisions.
- Open communication with your healthcare team regarding your concerns and treatment options is key.
- By understanding the diverse causes and available management strategies, you can breathe easier and reclaim a more comfortable life.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
RHINOSINUSISTIS
Delving into the Labyrinth: A Comprehensive Guide to Managing Rhinosinusitis
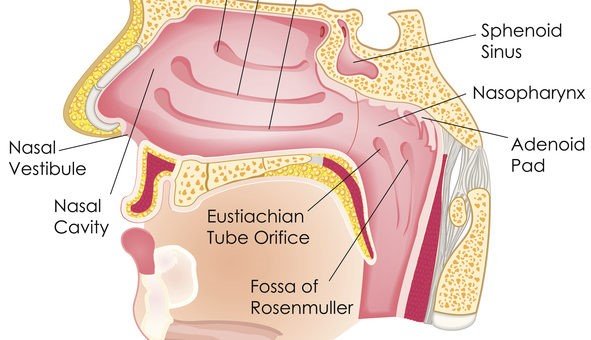
Rhinosinusitis, commonly known as sinusitis, involves inflammation of the sinuses and nasal passages, causing discomfort, pressure, and a host of other symptoms. This detailed summary explores the diverse causes, diagnosis, and various management options to help you navigate this condition effectively.
Unveiling the Culprits:
Types of sinusitis
For the duration of the symptoms
- Acute sinusitis – Last less than 4 weeks
- Normally infective (bacterial, fungal, or viral)
- Recurrent acute rhinosinusitis (RARS) ->4 episodes of acute sinusitis in a year
- Sub-acute sinusitis – Last between 1 to 3 months
- Chronic sinusitis (CRS) – Last for more than 3 months
Classifications of chronic rhinosinusitis
- Allergic fungal rhinosinusitis (AFRS)
- Rhinosinusitis with nasal polyps (CRSwNP) (30%)
- Rhinosinusitis without nasal polyps (CRPsNP) (70%)
(further subclassfication still on research)
Identifying the Problem:
Accurate diagnosis is crucial for tailoring treatment effectively. Consider:
- Detailed history: Discussing duration, severity, associated symptoms (nasal discharge, facial pain, fever), and potential triggers.
- Physical examination: Examining the nose, throat, and face for signs of inflammation, polyps, or structural issues.
- Nasal endoscopy: Visualizing the inside of the nasal passages using a thin, lighted tube.
- Imaging tests: CT scan to examine the sinuses in detail, particularly for chronic cases or suspected complications.
Tailoring Treatment to the Cause:
The approach depends on the identified cause and severity:
Acute Rhinosinusitis:
- Symptomatic relief: Over-the-counter pain relievers, decongestants (use cautiously), saline nasal irrigation, and rest.
- Antibiotics: Only for confirmed bacterial infections, not effective for viral causes.
- Nasal corticosteroids: Reduce inflammation, particularly in allergic cases.
Chronic Rhinosinusitis:
- Medications: Long-term nasal corticosteroids, antibiotics for specific situations, allergy medications.
- Nasal saline and irrigation: Essential for promoting drainage and reducing inflammation.
- Nasal polyp removal: Surgery to remove nasal polyps obstructing drainage.
- Balloon sinuplasty: Minimally invasive procedure to open blocked sinus passages.
- Functional endoscopic sinus surgery (FESS): More extensive surgery in complex cases.
Additional Considerations:
- Managing allergies: Identifying and avoiding triggers, using medication and immunotherapy if needed.
- Improving air quality: Using air purifiers and humidifiers, reducing exposure to smoke and dust.
- Lifestyle modifications: Getting enough sleep, managing stress, and drinking plenty of fluids.
Remember:
- Early diagnosis and proper management are crucial to prevent complications like facial cellulitis, meningitis, and vision problems.
- Different causes require different approaches, and individual factors influence treatment decisions.
- Open communication with your healthcare team regarding concerns and treatment options is key.
- By understanding the diverse causes and available management strategies, you can effectively manage rhinosinusitis and reclaim a healthier and more comfortable life.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
SMELL DISORDERS
Navigating the Labyrinth: Managing Smell Disorders in High Detail
Losing your sense of smell can be devastating, impacting your taste, enjoyment of life, and even safety. While a complete cure isn’t always possible, detailed management plans can significantly improve your olfactory function and quality of life. Here’s a comprehensive overview of managing smell disorders:
Understanding the Roots:
- Sinus Issues: Allergies, infections, and structural abnormalities like polyps can block airflow and affect smell perception. We offer:
- Allergy management: Medications, immunotherapy, and allergy shots.
- Sinusitis treatment: Antibiotics, saline irrigation, and minimally invasive surgery for polyps.
- Structural correction: Septoplasty or other surgical procedures to address anatomical issues.
- Head Injuries: Traumatic brain injuries can damage the olfactory nerve or olfactory centers in the brain. We provide:
- Neurological consultations: Working with neurologists to assess and manage related neurological conditions.
- Rehabilitation therapies: Occupational and speech-language therapy to address post-injury challenges.
- Neurological Conditions: Parkinson’s, Alzheimer’s, and other neurological disorders can impact smell. We offer:
- Collaborative care: Partnering with neurologists to manage your underlying condition and its impact on smell.
- Supportive measures: Nutritional counseling and other interventions to improve quality of life.
- CoVid infection: One of the initial presentations of CoVid, and lasting effects, is loss of the sense of smell. Most people recover the sense of smell in the first few months fter the infection, bur for a small number of patients the anosmia is permanent
- Medications: Certain medications can cause temporary smell loss. We offer:
- Medication review: Working with your primary care physician to identify and potentially switch medications.
- Management of side effects: Providing treatment options to minimize smell loss when medication change is not possible.
- Age-Related Decline: While natural, age-related decline can be addressed with:
- Smell training: Retraining your olfactory system to recognize and identify different scents.
- Nutritional counseling: Optimizing your diet to enhance taste and enjoyment of food.
Diagnosing the Culprit:
- Detailed History: Discussing your symptoms, medical history, potential triggers, and medication use.
- Physical Examination: Examining your nose and sinuses for abnormalities and signs of inflammation.
- Smell Tests: Standardized tests like Brief Smell Identification Test (BSIT) to measure odor identification and discrimination.
- Imaging Tests: CT scans or MRI scans to visualize your nasal structures and brain in complex cases.
Treatment Tailored to You:
- Medical Treatment: Addressing underlying conditions like allergies, infections, or neurological disorders with appropriate medications.
- Surgery: Minimally invasive procedures like sinus surgery or polyp removal to improve airflow and access to olfactory receptors.
- Smell Training: Regular exposure to specific sets of scents to stimulate olfactory neurons and retrain the brain.
- Olfactory Prosthetics: In rare cases, advanced devices like the “electronic nose” can directly stimulate the olfactory nerve.
- Supportive Measures: Nutritional counseling, support groups, and psychological support to cope with the emotional impact of smell loss.
Remember:
- Early diagnosis and management are crucial for maximizing improvement.
- Treatment success depends on the underlying cause and individual factors.
- While a complete cure may not always be possible, significant improvement in smell function and quality of life is achievable.
- Don’t hesitate to seek professional help from an experienced ENT specialist.
This summary provides a high-level overview. Consult with an ENT specialist for personalized diagnosis and treatment plan based on your unique situation.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
SNORING / SLEEP APNOEA
Managing Snoring and Sleep Apnoea: Restoring Your Sleep and Health
Snoring and sleep apnoea are widespread issues impacting millions, disrupting sleep quality and potentially leading to serious health consequences. Fortunately, a range of effective management strategies exist, tailored to both conditions and their diverse presentations. Here’s a comprehensive overview:
Understanding the Root Cause:
Snoring:
- Anatomical factors: Enlarged tonsils, adenoids, uvula, or a narrowed airway contribute to turbulent airflow and vibration, causing snoring.
- Muscle weakness: Relaxed throat muscles during sleep lead to tissue vibration and snoring.
- Lifestyle factors: Alcohol, sedatives, and overweight/obesity increase tissue laxity and worsen snoring.
Sleep Apnoea:
- Obstructive sleep apnoea (OSA): Most common type, where the airway repeatedly closes or narrows during sleep due to tissue collapse, causing breathing pauses (apneas) and reductions in oxygen levels (hypopneas).
- Central sleep apnoea (CSA): Less common, where the brain fails to send proper breathing signals, leading to apnoeas and hypopneas.
Diagnosing the Problem:
- Medical history and physical examination: Detailed discussion of symptoms, sleep habits, and risk factors, followed by an examination to assess potential anatomical contributors.
- Sleep study: Overnight study at home or in a sleep lab to monitor sleep stages, breathing patterns, oxygen levels, and other physiological parameters. This definitively diagnoses apnoea type and severity.
Treatment Approaches:
Lifestyle modifications:
- Weight loss: Even modest weight reduction can significantly improve both snoring and OSA.
- Positional therapy: Avoiding sleeping on the back can reduce airway closure in some OSA cases.
- Alcohol and sedative avoidance: These substances relax throat muscles and worsen both snoring and apnoea.
- Smoking cessation: Improves airway health and reduces inflammation, benefitting both conditions.
Medical Interventions:
- Continuous Positive Airway Pressure (CPAP): Gold standard for moderate to severe OSA, using a mask to deliver constant positive pressure to keep the airway open during sleep.
- Auto-Adjusting Positive Airway Pressure (APAP): Similar to CPAP, but adjusts pressure automatically throughout the night.
- Oral appliances: Customizable mouthpieces worn during sleep to reposition the jaw and tongue, opening the airway in mild to moderate OSA.
- Surgery: Various options, like uvulopalatopharyngoplasty (UPPP) or tonsillectomy, may be considered for specific anatomical contributors to snoring or mild OSA.
Addressing Snoring:
- Nasal dilators: Expand the nasal passages, improving airflow and reducing snoring in some cases.
- Nasal corticosteroids: Reduce inflammation in the nasal passages, potentially benefiting mild snoring.
- Radiofrequency ablation: Minimally invasive procedure to shrink tissue in the soft palate, reducing vibration and snoring.
Remember:
- Early diagnosis and management are crucial to prevent potential health complications of sleep apnea, like cardiovascular disease, stroke, and cognitive decline.
- Treatment choice depends on the type and severity of the condition, individual factors, and preferences.
- Regular follow-up with your healthcare provider is essential to monitor progress and adjust treatment as needed.
Remember, this is just a summary. Always consult with a qualified healthcare professional for personalized diagnosis and treatment planning based on your unique situation.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
Nose bleeds / Epistaxis
Managing Epistaxis: Stopping Nosebleeds Effectively
Nosebleeds, or epistaxis, are a common occurrence, particularly in the dry winter months. While usually harmless, severe or recurrent bleeding can be concerning and require medical attention. This summary explores the comprehensive management of epistaxis, ensuring accurate diagnosis and effective treatment.
Understanding the Culprit:
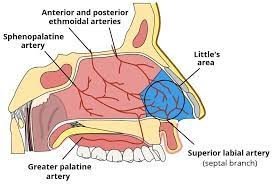
Epistaxis can originate from two main regions:
- Anterior epistaxis: 90% of cases, arising from the thin-walled blood vessels in the Kiesselbach plexus (Little’s area) located on the lower anterior septum.
- Posterior epistaxis: Less frequent, stemming from deeper branches of the internal maxillary artery within the back of the nasal cavity.
Identifying the Cause:
Several factors can trigger nosebleeds:
- Environmental: Dry air, allergies, nose-picking, sinusitis, and high altitude.
- Medical conditions: High blood pressure, blood thinners, liver disease, and clotting disorders.
- Trauma: Facial injury or nose surgery.
- Others: Cocaine use, hormonal changes during pregnancy, and certain medications.
Diagnosis and Assessment:
- Detailed history: Discussing medical history, recent trauma, medications, and bleeding characteristics (frequency, duration, and severity).
- Physical examination: Examining the nose for bleeding site, septal deviations, or foreign objects.
- Anterior rhinoscopy: Using a lighted instrument to visualize the anterior nasal cavity and pinpoint the bleeding source.
- Posterior rhinoscopy: In rare cases, with a flexible nasopharyngoscope to evaluate the posterior nasal cavity.
- Imaging: CT scan or angiography (rarely) to identify deeper vascular abnormalities.
Treatment Strategies:
Anterior Epistaxis:
- Direct pressure: Apply firm, continuous pressure to the soft part of the nose for 10-15 minutes, tilting the head forward to prevent blood ingestion.
- Nasal packing: Absorbent materials (merocellulose foam, tampons) inserted into the bleeding nostril to tamponade the vessel and promote clotting.
- Chemical cauterization: Silver nitrate or trichloroacetic acid applied to the bleeding point to seal the vessel.
- Electrical cauterization: Using controlled heat to seal the bleeding point (bipolar, laser).
- Anterior nasal packing: Balloon catheters or packs placed deeper in the nasal cavity for persistent bleeding.
Posterior Epistaxis:
- Posterior nasal packing: Specialized packs, balloons, or nasal tampons inserted beyond the choanae to compress the sphenopalatine artery.
- Embolization: Minimally invasive procedure where a catheter is guided through the arteries to the bleeding site to deliver clotting agents.
- Surgery: In rare cases, surgical ligation of the sphenopalatine artery is performed.
Post-Bleed Management:
- Humidification: Moist air prevents dryness and further irritation.
- Nasal saline sprays: Soften dry crusts and promote healing.
- Avoidance of nose-picking and strenuous activity.
- **Regular ** Monitor healing and address any underlying conditions.
Remember:
- Early diagnosis and prompt treatment are crucial to prevent complications like excessive blood loss, anemia, and even airway obstruction.
- Seeking medical attention for severe, recurrent, or persistent bleeding is crucial.
- Understanding the cause and implementing preventive measures can minimize the risk of future epistaxis.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation
Nasal polyps
In-Depth Management of Nasal Polyps: Breathing Easy Again
Nasal polyps can be frustrating and debilitating, impacting your ability to breathe, smell, and enjoy life. While a cure isn’t always possible, detailed management plans can significantly improve your symptoms and quality of life. Here’s a deep dive into managing nasal polyps:
Understanding the Roots:
- Chronic Inflammation: Allergies, recurring sinus infections, and asthma can create an inflammatory environment where polyps thrive.
- Structural Abnormalities: Deviated septum, narrow passages, and enlarged adenoids can trap irritants and promote polyp growth.
- Immune System Issues: Certain conditions like cystic fibrosis or Churg-Strauss syndrome can increase polyp risk.
- Other Contributors: Environmental factors like pollution, smoking, and occupational exposures might play a role.
Identifying the Culprit:
- Detailed History: Discussing symptoms, allergies, medical history, and environmental exposures.
- Physical Examination: Examining the nose and sinuses for polyps, inflammation, and structural issues.
- Nasal Endoscopy: Using a thin, flexible camera to directly visualize polyps and assess the nasal cavity and sinuses.
- Imaging Tests: CT scans or MRIs to determine polyp size, extent, and identify related anatomical problems.
Treatment Tailored to You:
- Medical Management: The cornerstone of treatment, aimed at reducing inflammation and shrinking polyps. Options include:
- Nasal Corticosteroids: Sprays or drops like fluticasone, budesonide, or mometasone are the first line of defense.
- Saline Irrigation: Regularly flushing the nasal passages with saltwater solution removes mucus, allergens, and irritants.
- Antihistamines and Decongestants: Offer temporary relief from allergy-related symptoms.
- Oral Corticosteroids: Short-term courses in severe cases or when nasal steroids are ineffective.
- Minimally Invasive Techniques: When medication isn’t enough, these options offer targeted relief:
- Balloon Sinuplasty: A catheter with a balloon tip dilates narrowed passages, improving drainage and access to polyps.
- Coblation Surgery: Uses radiofrequency energy to shrink polyps and open drainage pathways with minimal tissue damage.
- Surgical Intervention: Reserved for severe cases or recurrent polyps:
- Endoscopic Sinus Surgery (ESS): Minimally invasive procedure using thin instruments guided by an endoscope to remove polyps and restore sinus drainage.expand_more
- Traditional Sinus Surgery: More extensive surgery in complex cases or when ESS isn’t suitable.
Post-Treatment Care and Prevention:
- Continued Medication: Long-term use of nasal corticosteroids or other medications may be needed to prevent recurrence.
- **Regular ** Monitoring progress and adjusting treatment as needed is crucial.
- Addressing Underlying Causes: Managing allergies, asthma, or immune system issues can minimize polyp regrowth.
- Lifestyle Modifications: Avoiding irritants like smoke, pollution, and allergens; using a humidifier, and maintaining good hygiene may help.
Additional Considerations:
- Treatment success depends on: polyp size and location, severity of symptoms, underlying causes, and patient adherence to treatment.
- Choosing the right treatment: Discuss options with your doctor based on your individual needs and preferences.
- Emerging therapies: Research is ongoing to explore new options like biologics and immunotherapy for polyp management.
Remember:
- Early diagnosis and management are key to preventing complications like chronic sinusitis, sleep apnea, and anosmia (loss of smell).
- Don’t hesitate to seek professional help for persistent nasal symptoms.
- With the right approach, you can reclaim your breath and enjoy a better quality of life.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation
FACIAL PAIN
Navigating the Labyrinth: Managing Facial Pain in High Detail
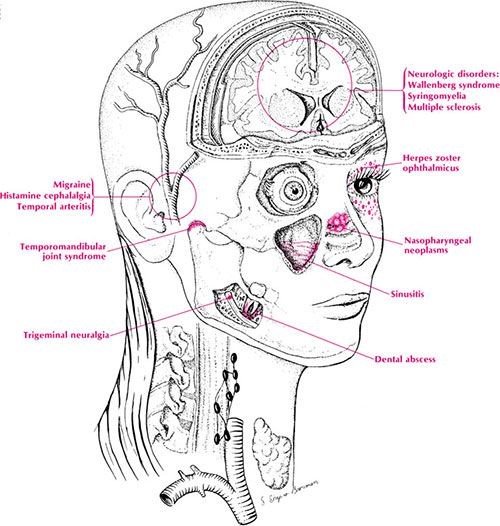
Facial pain can be a complex and challenging issue, encompassing a diverse range of conditions with equally diverse management strategies. This summary explores various approaches to tackle facial pain, empowering you to seek informed guidance and regain control of your well-being.
Understanding the Roots:
The path to managing facial pain begins with identifying its cause. This can be intricate, as numerous factors can be at play:
- Nerve-related: Trigeminal neuralgia, post-herpetic neuralgia, and other neuropathic conditions affect nerves themselves, causing burning, stinging, or electrical shock-like sensations.
- Musculoskeletal: Temporomandibular joint (TMJ) disorders, muscle tension headaches, and myofascial pain syndromes involve problems with jaw joints, muscles, and surrounding tissues, presenting with aching, dull pain.
- Dental issues: Toothaches, infections, and jaw problems can manifest as facial pain.
- Sinus issues: Inflammation in the sinuses can radiate pain to the face.
- Other conditions: Migraines, cluster headaches, and even psychological factors like stress and anxiety can contribute to facial pain.
Key Diagnostic Tools:
A multifaceted approach is essential for accurate diagnosis:
- Detailed history: Discussing your pain characteristics, location, triggers, and medical history.
- Physical examination: Examining your face, jaw, joints, and looking for signs of underlying conditions.
- Imaging tests: X-rays, CT scans, or MRIs may be used to visualize jaw joints, sinuses, and other structures.
- Nerve tests: Specialized tests might assess nerve function and pinpoint nerve-related issues.
Treatment Tailored to Your Needs:
The management plan depends on the underlying cause and your specific situation. Here are some potential approaches:
Medication:
- Pain relievers: Over-the-counter or prescription medications like NSAIDs or opioids can offer temporary relief for milder pain.
- Antidepressants: Certain antidepressants can be helpful for neuropathic pain and chronic pain syndromes.
- Anticonvulsants: Medications like gabapentin and carbamazepine are crucial for trigeminal neuralgia and other nerve-related pain.
- Muscle relaxants: May be used for TMJ disorders and muscle tension headaches.
Non-Medication Therapies:
- Physical therapy: Exercises, massages, and heat/cold therapy can improve joint mobility, muscle relaxation, and pain management.
- Cognitive-behavioral therapy (CBT): Can help manage stress, anxiety, and pain perception in chronic pain conditions.
- Acupuncture: May provide some pain relief, although evidence is mixed.
- Neurostimulation: Techniques like spinal cord stimulation or peripheral nerve stimulation can offer long-term pain relief in specific cases.
Addressing Underlying Issues:
- Dental treatment: Addressing toothaches, infections, or jaw problems can eliminate a pain source.
- Sinus treatment: Treating allergies or infections can alleviate sinus-related pain.
- Lifestyle modifications: Managing stress, getting enough sleep, and practicing good posture can contribute to pain reduction.
Surgical Intervention:
In rare cases, surgery may be considered:
- Trigeminal neuralgia: Procedures like radiofrequency ablation or microvascular decompression can target the affected nerve.
- TMJ disorders: Surgical interventions might address joint problems when conservative measures fail.
- Facial reconstruction: For severe facial injuries or structural issues.
Remember:
- Early diagnosis and proper management are crucial to prevent pain progression and improve quality of life.
- There is no “one-size-fits-all” solution. Treatment varies depending on the cause and individual factors.
- Open communication with your healthcare provider is key to finding the most effective approach for you.
- Consider attending support groups or seeking additional resources for emotional and practical support.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.