BIOPSY NECK MASS
Biopsy of a Neck Mass Under General Anaesthesia: A Deep Dive
A neck mass biopsy is a minimally invasive procedure used to diagnose the nature of a lump or swelling in the neck. This biopsy is performed under general anaesthesia to ensure patient comfort and minimize movement during the procedure. Here’s a detailed breakdown of the process:
Reasons for Neck Mass Biopsy:
There are various reasons why a doctor might recommend a biopsy of a neck mass:
- Diagnosis: The primary reason is to determine the cause of the mass. This could be an infection, benign growth (noncancerous), lymphoma (cancer of the lymphatic system), or another type of cancer.
- Treatment Planning: Knowing the exact nature of the mass helps guide treatment decisions. For example, a benign growth may require removal, while a cancerous mass might necessitate further treatment like surgery, radiation, or chemotherapy.
Pre-Operative Preparation:
Before the biopsy, your doctor will discuss your medical history, current medications, and any allergies you may have. Here are some typical pre-operative steps:
- Blood Tests: These may be done to assess your overall health and bleeding risk.
- Imaging Studies: An ultrasound, CT scan, or MRI scan might be used to visualize the mass and determine its size, location, and relationship to surrounding structures.
- Informed Consent: You will be asked to sign an informed consent form after understanding the risks and benefits of the procedure.
- Fasting Instructions: You may be advised to stop eating or drinking several hours before the surgery, depending on the type of anaesthesia used.
Procedure:
The biopsy is typically performed in an outpatient setting, meaning you can likely go home the same day after recovery from anaesthesia. Here’s a breakdown of the steps:
- Anaesthesia: General anaesthesia is administered through an intravenous (IV) line in your arm, allowing you to sleep comfortably throughout the procedure.
- Positioning: You’ll be positioned lying on your back with your head slightly tilted back.
- Sterilization: The area around the mass will be thoroughly cleaned and sterilized with an antiseptic solution.
- Anaesthetic Injection: A local anaesthetic may be injected at the biopsy site to numb the area further.
- Biopsy Technique: There are two main biopsy techniques used for neck masses:
- Fine-Needle Aspiration (FNA): A thin needle is inserted into the mass using ultrasound guidance to ensure accuracy. A small sample of cells is then withdrawn with a syringe for microscopic examination. FNA is a minimally invasive and preferred approach for most neck masses.
- Core Needle Biopsy: A larger needle is used to extract a core of tissue from the mass. This approach provides a larger sample for more definitive diagnosis, but it requires a slightly larger incision.
- Sample Handling: The extracted tissue or cells are carefully preserved and sent to a pathology lab for examination under a microscope by a pathologist who will determine the nature of the mass.
- Bandage Application: A small bandage will be applied to the biopsy site after stopping any bleeding.
Recovery:
- Post-Anaesthesia Care: You’ll be monitored in a recovery room until the effects of anaesthesia wear off.
- Pain Management: You may experience some soreness or discomfort at the biopsy site, which can be managed with pain medication.
- Biopsy Results: It typically takes a few days to receive the biopsy results from the pathology lab. Your doctor will discuss the findings with you and recommend the next steps based on the diagnosis.
Long-Term Considerations:
- Infection: There’s a slight risk of infection at the biopsy site. Watch for signs of infection like redness, swelling, fever, or pus drainage.
- Bleeding: Minor bleeding at the biopsy site is possible. Apply gentle pressure if needed.
- Bruising: Some bruising around the biopsy site can occur, which usually resolves on its own within a few days.
Benefits of a Biopsy:
- Accurate diagnosis: Provides vital information to guide treatment decisions.
- Early detection: Can help identify cancer at an early stage, improving treatment outcomes.
- Peace of mind: Knowing the nature of the mass can alleviate anxiety and uncertainty.
Remember:
- Biopsy of a neck mass is a valuable diagnostic tool with high accuracy.
- The specific procedure chosen depends on individual factors and potential benefits outweighing the risks.
- Open communication with your doctor throughout the process is crucial.
Overall, a neck mass biopsy under general anaesthesia is a safe and effective procedure for diagnosing the cause of a lump or swelling in the neck. Understanding the reasons for the biopsy, the procedure itself, and potential considerations can empower you to make informed decisions about your health.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
NECK DISSECTION
Neck Dissection: A Detailed Exploration of Lymph Node Removal in the Neck
A neck dissection is a surgical procedure designed to remove lymph nodes from the neck, often performed in conjunction with treatment for head and neck cancers. These cancers can originate in various structures of the head and neck region, including the oral cavity, pharynx, larynx, thyroid gland, and salivary glands. Lymph nodes play a crucial role in the immune system, but they can also be the first site where cancer cells spread from the primary tumour.
Why Perform a Neck Dissection?
There are two main reasons why a neck dissection might be recommended:
- Staging: In some cancers, such as head and neck cancers or melanoma (skin cancer), a neck dissection may be performed during the initial cancer diagnosis process. This helps determine the stage (extent) of cancer by assessing whether the lymph nodes in the neck contain cancer cells.
- Treatment: A neck dissection can be performed as a treatment for cancer that has already spread to the lymph nodes in the neck. Removing these involved lymph nodes helps eliminate potential reservoirs of cancer cells and improve overall treatment outcomes.
Types of Neck Dissection:
The extent of lymph node removal depends on the specific location of the primary tumour and the potential risk of lymph node involvement. Here’s a breakdown of the main types of neck dissection:
- Radical Neck Dissection: This removes all lymph nodes from one side of the neck, including the sternocleidomastoid muscle (large muscle in the neck), internal jugular vein (major vein), and spinal accessory nerve (controls neck movement). It’s the most extensive type of neck dissection.
- Modified Radical Neck Dissection: This is a less extensive procedure compared to the radical approach. It preserves some non-lymphatic structures like the sternocleidomastoid muscle or internal jugular vein.
- Selective Neck Dissection: This removes only the lymph nodes with the highest risk of containing cancer cells based on the location of the primary tumour. It’s the least extensive approach.
Pre-Operative Preparation:
Before surgery, a series of tests will be conducted to determine the extent of the surgery and assess your overall health. This may include:
- Imaging Studies: CT scans and PET scans can help identify the location and size of lymph nodes and assess potential spread of cancer.
- Fine-Needle Aspiration (FNA): A thin needle is inserted into a suspicious lymph node to withdraw a small sample of cells for microscopic examination to confirm the presence of cancer cells.
The Neck Dissection Procedure (Typically Inpatient Surgery):
The details of the procedure depend on the chosen type of neck dissection. Here’s a general overview:
Pre-Operative Assessment:
- Medical History and Physical Examination: The doctor will review your medical history, perform a physical examination focusing on the head and neck, and discuss the procedure in detail.
- Imaging Tests: CT scans or PET scans may be ordered to assess the primary tumour and potential lymph node involvement.
- Anaesthesia: General anaesthesia is typically used to keep the patient unconscious and comfortable during the surgery.
Surgical Steps:
- Anaesthesia Induction: General anaesthesia is administered.
- Incision: The surgeon makes an incision along the side of the neck, depending on the type of neck dissection.
- Muscle Dissection: Muscles in the neck may be partially or completely removed to access the lymph nodes.
- Lymph Node Removal: The surgeon carefully removes the targeted lymph node groups.
- Nerve Preservation (if possible): Efforts are made to preserve important nerves in the neck whenever possible, depending on the type of dissection.
- Closure: The incision is closed with stitches or staples.
- Drainage Tube Placement: A temporary drainage tube may be placed to remove excess fluids from the surgical site.
Recovery from Neck Dissection:
Recovery from a neck dissection can vary depending on the extent of the surgery. Generally, it involves:
- Hospital Stay: Neck dissection is typically an inpatient procedure, requiring a hospital stay for several days.
- Pain Management: Pain medication is provided to manage post-surgical discomfort.
- Physical Therapy: Exercises may be recommended to improve neck mobility and shoulder function.
- Dietary Modifications: Soft foods may be recommended initially, followed by a gradual return to a regular diet.
- Follow-up Appointments: Regular follow-up appointments are essential to monitor healing and check for any signs of infection or complications.
Potential Complications:
Neck dissection, like any surgery, carries potential risks and complications. These may include:
- Bleeding: Bleeding can occur during or after surgery.
- Infection: There’s a risk of infection at the surgical site.
- Lymphedema: This is a build-up of fluid in the arm or face due to damage to the lymphatic system.
- Nerve Injury: Damage to nerves in the neck can cause weakness, numbness, or pain.
- Wound Healing Problems: The incision site may take longer than expected to heal.
Conclusion:
Neck dissection is a vital component of head and neck cancer treatment. While it can be a complex surgery, it offers the potential to improve survival rates and overall outcomes. If you’re facing head and neck cancer treatment, discuss the possibility of a neck dissection with your doctor to understand if it’s part of your recommended treatment plan
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
BRACHIAL CLEFT CYST EXCISION
Brachial Cyst Excision: Removing a Benign Neck Mass
A brachial cyst excision is a surgical procedure designed to remove a brachial cleft cyst, a benign (noncancerous) congenital mass that develops in the neck or upper chest. These cysts arise from remnants of embryonic tissue left behind during foetal development. While typically harmless, they can cause cosmetic concerns or discomfort if they become large enough.
Why Perform Brachial Cyst Excision?
There are several reasons why a doctor might recommend an excision of a brachial cyst:
- Cosmesis: Brachial cleft cysts can be visible as a lump on the neck or upper chest, leading to cosmetic concerns for some individuals.
- Discomfort: Large cysts can press on surrounding structures, causing pain or discomfort.
- Infection: Although uncommon, cysts can become infected, leading to redness, swelling, and tenderness.
- Rapid Growth: Rapidly growing cysts warrant investigation and may be recommended for removal.
Who is a Candidate for Brachial Cyst Excision?
Brachial cyst excision is typically considered for individuals experiencing:
- Significant cosmetic concerns due to the cyst’s appearance.
- Pain or discomfort caused by the cyst pressing on surrounding structures.
- Signs of infection within the cyst.
- Rapid growth of the cyst.
Types of Brachial Cysts:
There are four types of brachial cleft cysts, classified based on their location:
- First Branchial Cleft Cyst: Located near the earlobe or angle of the jaw, sometimes associated with a preauricular pit (a small skin depression near the ear).
- Second Branchial Cleft Cyst: Developing just below the angle of the jaw, sometimes with a draining sinus tract (a narrow channel) leading to the skin surface.
- Third Branchial Cleft Cyst: Found on the side of the neck, occasionally involving the thyroid gland or parathyroid gland.
- Fourth Branchial Cleft Cyst: Located behind the sternocleidomastoid muscle (large muscle in the neck), sometimes near the collarbone.
The type of brachial cleft cyst can influence the surgical approach.
The Brachial Cyst Excision Procedure (Typically Outpatient Surgery):
The details of the procedure depend on the cyst’s location and size. Here’s a general breakdown:
Pre-Operative Assessment:
- Medical History and Physical Examination: The doctor will review your medical history, perform a physical examination focusing on the neck and chest, and discuss the procedure.
- Imaging Tests: Ultrasound or CT scan may be ordered to assess the cyst’s size, location, and relationship to surrounding structures.
- Anaesthesia: The type of anaesthesia used depends on the complexity of the surgery. Local anaesthesia with sedation or general anaesthesia may be used.
Surgical Steps:
- Anaesthesia Induction: Local anaesthesia with sedation or general anaesthesia is administered for patient comfort.
- Incision: The surgeon makes an incision over the cyst, considering the cyst’s location and minimizing scar visibility.
- Cyst Dissection: The surgeon carefully dissects the cyst from surrounding tissues, ensuring complete removal of the cyst wall. This minimizes the risk of recurrence.
- Bleeding Control: Any bleeding is controlled using cautery (heat) or other methods.
- Closure: The incision is closed with stitches or staples.
- Drainage Tube Placement (optional): In some cases, a temporary drainage tube may be placed to remove excess fluids from the surgical site.
Recovery from Brachial Cyst Excision:
Recovery from brachial cyst excision is usually quick and involves:
- Hospital Stay: This is often an outpatient procedure, allowing you to return home the same day.
- Pain Management: Pain medication is provided to manage post-surgical discomfort.
- Scar Care: Following doctor’s instructions for wound care and scar management is essential.
- Follow-up Appointment: A follow-up appointment with the doctor is scheduled to monitor healing and remove stitches if used.
Potential Complications:
Brachial cleft cyst excision is a relatively safe procedure, but potential complications include:
- Bleeding: Bleeding can occur during or after surgery.
- Infection: There’s a risk of infection at the surgical site.
- Nerve Injury: Damage to nerves in the neck, although uncommon, can cause weakness, numbness, or pain.
- Scarring: While efforts are made to minimize scarring, some degree of scarring is possible.
- Cyst Recurrence: In rare cases, the cyst may recur if not completely removed.
Conclusion:
Brachial cyst excision is a safe and effective procedure for removing these
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
TRACHEOSTOMY
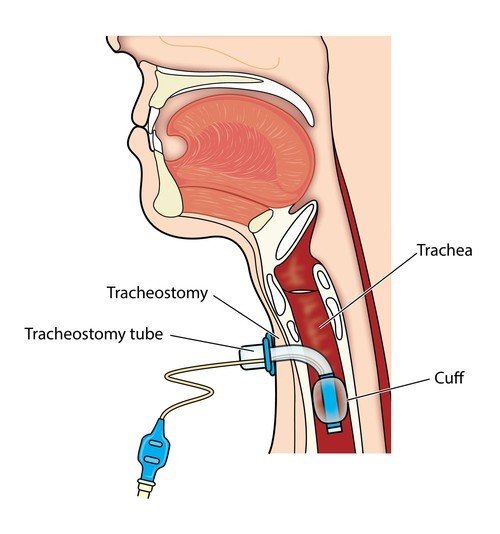
Tracheostomy: A Detailed Exploration
A tracheostomy is a surgical procedure that creates a temporary or permanent opening in the trachea (windpipe) through the neck. This opening, called a stoma, allows air to bypass the natural upper airway (nose and mouth) and enter the lungs directly. While often associated with critical care situations, tracheostomies have a wider range of applications.
Reasons for Tracheostomy:
- Respiratory Failure: This is the most common reason for a tracheostomy. It’s performed when a patient experiences severe breathing difficulties due to conditions like chronic obstructive pulmonary disease (COPD), neuromuscular diseases affecting breathing muscles, or upper airway obstruction caused by infections, tumours, or trauma. A tracheostomy ensures a secure and unobstructed airway for mechanical ventilation support.
- Prolonged Mechanical Ventilation: Patients requiring long-term mechanical ventilation (weeks or months) may benefit from a tracheostomy for comfort and improved patient care. It allows easier removal of secretions, reduces the risk of aspiration (inhaling fluids or food particles), and facilitates communication with the patient.
- Speech Impairment: In situations where a patient has undergone surgery on the face, mouth, or throat that affects their ability to speak or breathe normally, a tracheostomy can provide a temporary or permanent airway while allowing the upper airway to heal.
- Aspiration Prevention: For patients with swallowing difficulties or weak coughing reflexes who are at high risk of aspirating fluids or food particles into the lungs, a tracheostomy can help prevent aspiration pneumonia.
Types of Tracheostomy:
There are two main types of tracheostomies, each with different purposes and placement techniques:
- Surgical Tracheostomy: This is a planned procedure performed in a sterile operating room under general anaesthesia. The surgeon makes an incision in the neck, locates the trachea, and creates a stoma by inserting a tracheostomy tube. The specific type of tube and its placement (high or low on the trachea) depend on the patient’s needs.
- Percutaneous Dilation Tracheostomy (PDT): This is a less invasive procedure typically performed in an intensive care unit (ICU). After local anaesthesia, a guidewire is inserted through a small needle puncture in the neck to reach the trachea. A balloon is then inflated to create a pathway, and a tracheostomy tube is inserted.
Procedure and Recovery:
The details of the procedure will vary depending on the type of tracheostomy performed. Here’s a general overview:
- Surgical Tracheostomy:
- General anaesthesia ensures patient comfort and immobility during surgery.
- An incision is made in the neck, and the surgeon carefully locates and exposes the trachea.
- A stoma is created by opening the trachea, and a tracheostomy tube is inserted and secured to maintain the opening.
- The wound is closed around the tube, and a dressing is applied.
- Percutaneous Dilation Tracheostomy (PDT):
- Local anaesthesia numbs the area for patient comfort.
- A small needle is inserted through the skin and into the trachea under fluoroscopic guidance (real-time X-ray imaging).
- A guidewire is then inserted through the needle, followed by balloon dilation to create a pathway.
- A tracheostomy tube is inserted over the guidewire and secured.
- The area is cleaned and dressed.
Post-Operative Care:
- Hospital Stay: The length of hospital stay after a tracheostomy varies depending on the underlying condition and the patient’s recovery progress.
- Stoma Care: Learning proper stoma care and hygiene is crucial to prevent infection. This includes cleaning the stoma site regularly, changing the inner tube as prescribed, and managing secretions effectively.
- Breathing Support: Depending on the patient’s needs, mechanical ventilation may continue through the tracheostomy tube or may be weaned gradually as their breathing improves.
- Speaking: While a tracheostomy allows air to bypass the vocal cords, speech is typically not possible. However, some patients with tracheostomies can learn alternative communication methods like using a speaking valve attached to the tracheostomy tube or electronic communication devices.
- Rehabilitation: Speech therapy and occupational therapy can play a vital role in helping patients with tracheostomies regain communication skills, swallowing function, and independence with activities of daily living.
- Decannulation: In some cases, once the underlying condition improves, and the patient can breathe adequately on their own, the tracheostomy tube can be removed (decannulated). The stoma may close naturally, or in some cases, surgical closure may be necessary.
Long-Term Considerations:
- Stoma Care: Meticulous stoma care is essential to prevent infection. This includes daily cleaning, regular inner tube changes, and effective secretion management. Trained healthcare professionals will provide education and support.
- Breathing Support: The goal is to transition patients to breathe independently. Depending on their needs, mechanical ventilation may continue or be gradually weaned.
- Speaking: Speech is typically not possible due to bypassed vocal cords. Speech therapy can help explore alternative communication methods like speaking valves or electronic devices.
- Rehabilitation: Speech and occupational therapy can help regain communication skills, swallowing function (if affected), and independence in daily living.
- Decannulation: In some cases, the tracheostomy tube can be removed (decannulated) if the underlying condition improves, and the patient can breathe adequately on their own. The stoma may close naturally, or surgical closure may be necessary.
- Social and Emotional Considerations: Body image, communication challenges, and social interaction can be impacted. Support groups, counselling, and learning to manage the tracheostomy can help with adjustment.
- Quality of Life: Maintaining independence, strong social support networks, access to specialized healthcare, and emotional well-being are crucial for a good quality of life.
Additional Considerations:
- End-of-Life Care: Discussions about preferences regarding ventilation and tracheostomy management are important for patients with permanent tracheostomies.
- Advance Directives: Having advance directives in place ensures wishes regarding care are respected if incapacitated.
By understanding the long-term implications and available support systems, patients with tracheostomies can lead fulfilling and active lives.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
LARYNGECTOMY
Laryngectomy: A Deep Dive
What is a Laryngectomy?
A laryngectomy is a surgical procedure that involves removing all or part of the larynx, commonly known as the voice box. This complex surgery is primarily used to treat laryngeal cancer, but can also be necessary in other situations.
Reasons for Laryngectomy:
- Laryngeal Cancer (Primary Reason): Laryngectomy is often the chosen course of action when laryngeal cancer has become advanced or hasn’t responded well to other treatments like radiation or chemotherapy. The extent of the cancer and its location within the larynx determine the type of laryngectomy performed.
- Severe Trauma: Extensive injuries to the larynx due to accidents, gunshot wounds, or other forceful events may necessitate laryngectomy to preserve life and prevent further complications.
- Severe Laryngeal Disease: In rare cases, severe benign (non-cancerous) conditions affecting the larynx, such as chronic infections or airway obstructions that significantly impact breathing, might require laryngectomy as a last resort.
Types of Laryngectomy:
There are three main types of laryngectomies, each with varying degrees of tissue removal and subsequent impact on voice function and breathing:
- Total Laryngectomy: This is the most extensive procedure, involving the complete removal of the entire larynx, including the vocal cords. It results in a permanent loss of natural voice function.
- Supraglottic Laryngectomy: This is a less common procedure where only the upper portion of the larynx is removed. While some vocal function may be preserved, it’s often limited or altered.
- Partial Laryngectomy: This is the least common and most complex procedure, aiming to remove only the diseased portion of the larynx while preserving as much healthy tissue and function as possible. It may offer some degree of voice preservation, but the specific outcome depends on the extent of tissue removed.
Surgical Procedure:
Laryngectomy is a major surgery performed under general anaesthesia. The specific surgical approach depends on the type of laryngectomy being performed. Here’s a general breakdown:
- Incision: The surgeon makes an incision either in the neck (vertical or horizontal) or through the mouth (transoral approach). The choice depends on the location and extent of the cancer or other condition.
- Laryngeal Removal: The surgeon carefully removes the designated portion of the larynx, ensuring complete removal of cancerous tissue in cases of cancer.
- Stoma Creation: A permanent opening is created in the trachea (windpipe) called a stoma. This allows air to enter the lungs for breathing since the natural passage through the larynx is bypassed. Depending on the location of the stoma (high or low on the neck), a tracheostomy tube might be inserted initially to help with breathing during recovery and later potentially be replaced with a permanent stoma button.
- Reconstruction (Optional): In some cases, depending on the remaining tissue and goals of surgery, the surgeon may attempt reconstruction to improve swallowing function or even limited voice production.
Recovery and Long-Term Considerations:
- Hospital Stay: Following surgery, you will likely stay in the hospital for several days for monitoring, pain management, and initial recovery steps.
- Breathing: You will breathe entirely through the stoma after surgery. This may require using a special filter to prevent dust, moisture, and irritants from entering the lungs. Learning proper stoma care and hygiene is crucial to avoid infections.
- Speaking: Losing the voice box eliminates the ability to speak in the traditional way. However, several options can help regain communication skills:
- Oesophageal Speech: By learning to swallow air and control its release, you can create sounds in the oesophagus that can be formed into speech with practice and training.
- Electrolarynx: This handheld device held against the throat creates vibrations that are transmitted through the mouth and can be used to produce electronic speech.
- Speech Prosthesis: A surgically implanted device allows air to flow from the trachea to the oesophagus, enabling some natural-sounding speech in select cases.
- Swallowing: Laryngectomy may initially affect swallowing due to altered anatomy. Speech therapy plays a vital role in relearning swallowing techniques and regaining optimal function.
- Psychological Adjustment: Laryngectomy can be a life-altering experience. Emotional
Living After Laryngectomy:
- Long-Term Care: Regular follow-up visits with your doctor are essential to monitor your health, address potential complications (infection, stoma issues), and ensure proper stoma care.
- Adjustments and Support: Life after laryngectomy requires significant adjustments. Support groups connect patients with others who understand the challenges and offer valuable guidance and emotional support.
- Quality of Life: While communication and swallowing may require new approaches, people who have undergone laryngectomy can lead fulfilling lives with proper rehabilitation and support.
Additional Considerations:
- Psychological Impact: The loss of voice and physical changes can be emotionally challenging. Counselling services may be beneficial in coping with these adjustments.
- Long-Term Care: Regular follow-up with doctors is essential to monitor the stoma and overall health.
Additional Considerations:
- Laryngectomy is a complex surgery with potential risks and complications like bleeding, infection, and difficulty swallowing. Discussing these risks and potential side
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
TRANS-ORAL ROBOTIC SURGERY (TORS)
Transoral Robotic Surgery (TORS): A Minimally Invasive Approach to Head and Neck Cancer
Transoral Robotic Surgery (TORS) is a cutting-edge surgical technique that utilizes a robotic system to perform minimally invasive surgery through the mouth for accessing and treating tumours in the head and neck region. This approach offers several advantages over traditional open surgery, making it a valuable tool for treating a variety of cancers.
Applications of TORS:
- Tumour Sites: TORS can be used to treat tumours in various locations within the head and neck, including:
- Tongue
- Tonsils
- Larynx (voice box)
- Pharynx (throat)
- Base of the skull
- Cancer Types: TORS is particularly suitable for early-stage oropharyngeal cancers (cancers of the tonsils and base of the tongue) caused by the Human Papillomavirus (HPV). It can also be used for some other head and neck cancers in select cases.
Benefits of TORS:
- Minimally Invasive: Compared to traditional open surgery, TORS utilizes smaller incisions made within the mouth or neck. This leads to several advantages:
- Less pain and discomfort after surgery
- Faster recovery times
- Reduced blood loss during surgery
- Improved cosmetic outcomes with minimal scarring
- Enhanced Precision: The robotic system provides the surgeon with several benefits:
- 3D Visualization: High-resolution 3D magnified views of the surgical field allow for more precise dissection and tumour removal.
- Improved Dexterity: The robotic arms offer greater manoeuvrability and control within the confined spaces of the head and neck, enabling delicate procedures with minimal tissue damage.
Procedure:
- General Anaesthesia: The patient receives general anaesthesia to ensure comfort and immobility during surgery.
- Mouth Access: A surgical retractor is inserted through the mouth to widen the opening and provide the surgeon with a clear view of the surgical site.
- Robotic Arm Placement: Small incisions are made in the mouth or neck to allow for the insertion of the robotic arms. These arms are attached to surgical instruments that the surgeon controls from a console near the operating room.
- Surgery: The surgeon manipulates the robotic arms and instruments to perform the following:
- Dissect surrounding tissues
- Remove the tumour with minimal margin
- Perform any necessary reconstruction (depending on the location and size of the tumour)
- Closure: Once the surgery is complete, the retractor and robotic arms are removed. The small incisions are then closed with sutures.
Recovery:
- Hospital Stay: The length of stay depends on the complexity of the surgery and the patient’s recovery progress. Typically, patients stay for a few days for monitoring and pain management.
- Pain Management: Patients may experience some pain and soreness after surgery, which can be controlled with medication.
- Feeding: Depending on the location and size of the tumour removed, a feeding tube may be needed for a short period while swallowing recovers. Speech therapy may be recommended to help patients regain swallowing function and potentially improve speech clarity if affected.
Considerations:
- Suitability: TORS is not suitable for all head and neck cancers. The surgeon will carefully evaluate the size, location, and type of tumour to determine if TORS is the most appropriate approach. Other factors like the patient’s overall health and anatomy are also considered.
- Risks: As with any surgery, TORS carries potential risks, although these are generally less frequent compared to traditional open surgery. Potential risks include:
- Bleeding
- Infection
- Nerve injury
- Leakage of saliva
Overall, Transoral Robotic Surgery (TORS) offers a minimally invasive and potentially more precise approach to treating head and neck cancers. It can benefit patients by reducing recovery time, minimizing pain, and improving cosmetic outcomes. However, it’s important to discuss the suitability of TORS with your doctor to determine if it’s the right option for your specific situation.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
THYROIDECTOMY
Thyroidectomy: A Deep Dive into Thyroid Gland Removal
A thyroidectomy is a surgical procedure that removes all or part of the thyroid gland, located in the front of your neck just below the Adam’s apple. This gland produces hormones essential for regulating metabolism, growth, and development. While often performed to treat thyroid cancer, thyroidectomy has various applications.
Reasons for Thyroidectomy:
- Thyroid Cancer: The most common reason for a thyroidectomy is to remove cancerous or potentially cancerous growths in the thyroid gland. Early detection and removal of thyroid cancer are crucial for successful treatment and improving long-term outcomes.
- Thyroid Nodules: These are lumps in the thyroid that can be benign (noncancerous) or malignant (cancerous). A fine-needle aspiration biopsy will determine the nature of the nodule, and a thyroidectomy may be recommended for suspicious or large nodules.
- Graves’ Disease: This autoimmune disorder causes the thyroid to produce an excessive amount of thyroid hormone (hyperthyroidism). In some cases, medication or radioactive iodine therapy may not be effective, and a thyroidectomy becomes necessary.
- Hashimoto’s Thyroiditis: This is an autoimmune condition that leads to inflammation and eventual underproduction of thyroid hormone (hypothyroidism). Large goiters (enlarged thyroid glands) associated with Hashimoto’s may require thyroidectomy for management.
- Hyperthyroidism: In severe cases of hyperthyroidism not controlled by medication or radioactive iodine therapy, a thyroidectomy may be performed.
Types of Thyroidectomy:
- Total Thyroidectomy: Complete removal of the entire thyroid gland. This is the most common type performed for thyroid cancer.
- Near-Total Thyroidectomy: Removal of most of the thyroid gland, leaving a small amount of tissue intact. This may be an option for some types of thyroid cancer or large goitres.
- Hemithyroidectomy: Removal of one lobe of the thyroid gland. This may be performed for a small cancerous nodule on one side or a non-cancerous goitre affecting only one lobe.
The Thyroidectomy Procedure:
- Preparation: Performed under general anaesthesia in a hospital setting.
- Incision: The surgeon makes a small horizontal incision in the lower neck, strategically placed to minimize scarring.
- Muscle Separation: The surgeon carefully separates thin muscle layers to access the thyroid gland.
- Thyroid Tissue Removal: Depending on the type of thyroidectomy, either the entire gland, a portion of it, or one lobe is removed. Nearby lymph nodes may also be removed if there’s a concern about cancer spread.
- Haemostasis: Careful attention is paid to controlling bleeding throughout the procedure.
- Closure: The muscle layers and skin are stitched or closed with surgical glue.
Recovery and Follow-Up:
- Hospital Stay: Typically, patients stay for 1-2 nights for monitoring and pain management.
- Pain Management: Pain medication is prescribed to manage post-surgical discomfort.
- Scar Care: Instructions are provided on caring for the incision to minimize scarring.
- Hormone Replacement Therapy (HRT): Since the thyroid gland is no longer producing hormones, most patients will require lifelong hormone replacement therapy with synthetic thyroid hormone medication.
- Follow-Up Appointments: Regular check-ups with the doctor are crucial to monitor hormone levels and overall health.
- Calcium Monitoring: There’s a small risk of damage to the parathyroid glands located near the thyroid during surgery. These glands regulate calcium levels, so monitoring might be necessary to ensure proper calcium balance.
Potential Complications of Thyroidectomy:
- Infection: As with any surgery, there’s a risk of infection at the incision site.
- Bleeding: Bleeding during or after surgery can occur, though usually controlled by the surgeon.
- Hoarseness: Temporary hoarseness can occur due to irritation of the nerves controlling the vocal cords. In rare cases, permanent hoarseness might develop.
- Hypoparathyroidism: Damage to the parathyroid glands can lead to low calcium levels, requiring medication.
- Thyroid Crisis (Rare): If too much thyroid tissue is removed unintentionally, a life-threatening thyroid crisis can develop. However, this is uncommon with proper surgical techniques.
Living After Thyroidectomy:
- Most patients experience a significant improvement in symptoms related to thyroid problems after surgery.
- Regular monitoring and medication adherence are crucial for long-term health.
- Most people can resume normal activities within a few weeks after surgery.
Additional Considerations:
- Thyroid Cancer and Follow-Up: For patients who undergo thyroidectomy for thyroid cancer, additional treatment like radioactive iodine ablation or radioactive therapy might be needed depending on the specific type and stage of cancer. Regular follow-up with an endocrinologist is essential for monitoring cancer recurrence.
- Emotional Adjustment: Some patients may experience emotional challenges after surgery, especially those who lose their voice or have difficulty adjusting to lifelong medication. Support groups or counselling can be beneficial.
Remember: This summary provides a general overview. Consulting a doctor or endocrinologist is crucial to understand the specifics of thyroidectomy, its potential risks and benefits, and the recovery process tailored to individual cases.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
THYROGLOSSAL CYST SURGERY (SISTRUNK’S PROCEDURE)
TThyroglossal Duct Excision: Removing a Persistent Embryonic Structure
A thyroglossal duct excision is a surgical procedure to remove a thyroglossal duct remnant. The thyroglossal duct is a temporary structure present in the developing embryo that guides the thyroid gland from its initial location near the base of the tongue to its final position in the lower neck. In most cases, this duct disappears before birth. However, sometimes remnants of the duct persist, and this can lead to the formation of a thyroglossal duct cyst.
Reasons for Thyroglossal Duct Cyst Excision:
- Cosmesis: The primary reason for removal is often the unsightly appearance of the cyst in the neck.
- Discomfort: Large cysts can become uncomfortable or cause pressure on surrounding structures.
- Infection: While uncommon, a cyst can become infected, causing redness, pain, and swelling.
- Risk of Rupture: Though rare, a cyst can rupture, spilling its contents and potentially causing inflammation.
- Potential risk of malignant transformation: Though extremely rare, the cyst has a potential of long-term malignant transformation if is left untreated.
Pre-Operative Evaluation:
Before surgery, some tests might be performed to confirm the diagnosis and plan the surgical approach:
- Ultrasound: This imaging test helps visualize the cyst and assess its size, location, and any surrounding structures.
- Thyroid Scan (Optional): In some cases, a thyroid scan might be done to ensure the normal thyroid gland is functioning properly and separate from the cyst.
The Thyroglossal Duct Cyst Excision Procedure:
- Preparation: Performed under general anaesthesia (patient asleep) or local anaesthesia with sedation (numbs the area) in a hospital setting.
- Incision: The surgeon makes a horizontal incision directly over the cyst, strategically placed to minimize scarring.
- Dissection: The surgeon carefully dissects through skin and muscle layers to expose the cyst.
- Excision: The entire cyst sac, along with the thyroglossal duct tract leading down to the base of the tongue (the Sistrunk procedure), is meticulously removed to minimize the risk of recurrence.
- Haemostasis: Careful attention is paid to controlling any bleeding throughout the procedure.
- Closure: The muscle layers and skin are stitched or closed with surgical glue.
Benefits of the Sistrunk Procedure:
- Reduced Recurrence Rate: Removing the entire thyroglossal duct tract significantly reduces the risk of the cyst coming back compared to simpler excision methods.
Recovery and Follow-Up:
- Hospital Stay: Typically, patients stay for a few hours or overnight for monitoring and pain management.
- Pain Management: Pain medication is prescribed to manage post-surgical discomfort.
- Scar Care: Instructions are provided on caring for the incision to minimize scarring.
- Follow-Up Appointments: Regular check-ups with the doctor are essential to monitor the incision site and ensure proper healing.
Potential Complications of Thyroglossal Duct Cyst Excision:
- Infection: As with any surgery, there’s a risk of infection at the incision site.
- Bleeding: Bleeding during or after surgery can occur, though usually controlled by the surgeon.
- Bruising and Swelling: Temporary bruising and swelling around the incision area are common.
- Numbness: Temporary numbness around the incision site can occur due to nerve irritation. This typically resolves over time.
- Scarring: While scarring is inevitable, proper wound care can minimize its appearance.
- Recurrence: While uncommon with the Sistrunk procedure, there’s a slight risk of the cyst recurring if the entire tract is not removed.
Living After Thyroglossal Duct Cyst Excision:
- Most patients experience significant improvement in the appearance and comfort of their neck after surgery.
- Following post-operative instructions and attending follow-up appointments are crucial for optimal healing.
- Most people can resume normal activities within a few days or a week after surgery.
Additional Considerations:
- Minimally Invasive Techniques: In some cases, a minimally invasive surgical approach using endoscopic techniques might be an option. However, this is less common and may not be suitable for all patients.
- Thyroid Function: The surgery itself does not affect thyroid function. However, it’s important to ensure the normal thyroid gland is functioning properly before surgery.
Remember: This summary provides a general overview. Consulting an otolaryngologist (ENT doctor) is crucial to understand the specifics of your situation, the surgical approach recommended, and the recovery process tailored to your individual case.
PARATHYROIDECTOMY
Delving Deep into Parathyroidectomy: Understanding the Procedure
Parathyroidectomy is a surgical procedure that removes one or more parathyroid glands. These small glands, located behind the thyroid gland in the neck, are responsible for producing parathyroid hormone (PTH), which regulates calcium levels in the blood. Parathyroidectomy becomes necessary when the parathyroid glands become overactive and produce excessive PTH, leading to a condition called hyperparathyroidism.
Reasons for Parathyroidectomy:
- Primary Hyperparathyroidism: This is the most common reason, where the parathyroid glands themselves become enlarged and hyperactive, causing excessive PTH production.
- Secondary Hyperparathyroidism: Develops as a consequence of another medical condition, like chronic kidney disease, leading to overproduction of PTH by the parathyroids in an attempt to compensate for low calcium levels. However, surgery is typically not the first-line treatment here.
Symptoms of Hyperparathyroidism:
Hyperparathyroidism can cause a variety of symptoms, including:
- Bone pain and fractures due to weakened bones
- Kidney stones
- Fatigue
- Lethargy
- Depression
- Difficulty concentrating
- Nausea and vomiting
- Abdominal pain
Types of Parathyroidectomy:
- Minimally Invasive Parathyroidectomy (MIP): The preferred approach whenever possible. This technique uses smaller incisions and advanced visualization techniques to locate and remove the abnormal parathyroid gland(s) with minimal disruption to surrounding tissues.
- Open Parathyroidectomy: A more traditional approach involving a larger incision in the neck to access the parathyroid glands for exploration and removal. This may be necessary if the location of the abnormal gland(s) is unclear or if there are multiple enlarged glands.
Pre-Operative Evaluation:
Before surgery, various tests help identify the location and number of abnormal parathyroid glands:
- Blood tests: Measure calcium, PTH, and other electrolytes.
- Imaging tests: Techniques like ultrasound, sestamibi scan, or PET scan help pinpoint the abnormal parathyroid gland(s).
The Parathyroidectomy Procedure (Minimally Invasive):
- Preparation: Performed under general anaesthesia in an outpatient setting or hospital.
- Small Incisions: One or two small incisions are made in the neck.
- Localization Techniques: Imaging techniques like ultrasound or a tiny camera are used to precisely locate the abnormal parathyroid gland.
- Gland Removal: The surgeon removes the identified parathyroid gland using specialized surgical instruments.
- Blood Sample and PTH Check: During surgery, a blood sample is drawn to measure PTH levels in real-time. If PTH levels fall significantly after removing the first gland, it indicates a successful removal of the source of excess PTH.
- Closure: The incisions are closed with stitches or surgical glue.
Recovery and Follow-Up:
- Hospital Stay: Typically, patients go home the same day or stay overnight for observation in minimally invasive surgery cases.
- Pain Management: Pain medication is prescribed to manage post-surgical discomfort.
- Scar Care: Instructions are provided for incision care to minimize scarring.
- Follow-Up Appointments: Regular check-ups with the doctor are crucial to monitor calcium levels and ensure proper healing.
Benefits of Minimally Invasive Parathyroidectomy:
- Smaller incisions: Leads to less scarring and quicker recovery.
- Reduced pain: Minimally invasive techniques generally cause less post-surgical pain.
- Faster recovery: Patients can typically resume normal activities sooner compared to open surgery.
Potential Complications of Parathyroidectomy:
- Bleeding: As with any surgery, there’s a risk of bleeding during or after surgery.
- Infection: Infection at the incision site is a potential complication.
- Hypocalcaemia: Temporary low calcium levels can occur after surgery, usually managed with calcium supplements. In rare cases, it can be long-term.
- Recurrent Hyperparathyroidism: In rare instances, the surgery may not be curative, and hyperparathyroidism may recur.
Living After Parathyroidectomy:
- Most patients experience significant improvement in symptoms and a return to normal calcium levels after successful surgery.
- Calcium monitoring and medication: Long-term monitoring of calcium levels and possible calcium or vitamin D supplementation might be necessary.
- Return to normal activities: Most people can resume normal activities within a few days or a week after minimally invasive surgery.
Additional Considerations:
- Diagnosis: Accurate pre-operative localization of the abnormal parathyroid gland(s) is crucial for successful minimally invasive surgery.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
PAROTIDECTOMY
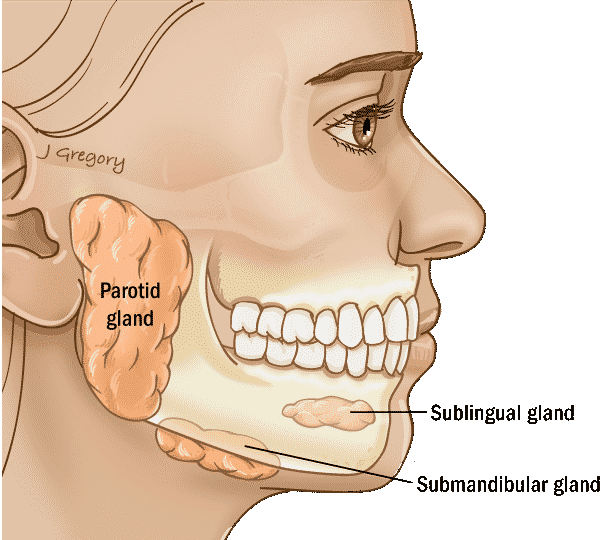
Unveiling Parotidectomy: A Deep Dive into Parotid Gland Removal
The parotid glands, located on either side of the face just below and in front of the ears, are major salivary glands responsible for producing saliva. Parotidectomy is a surgical procedure that removes all or part of one or both parotid glands. This surgery becomes necessary when dealing with parotid gland issues like tumours or other abnormalities.
Reasons for Parotidectomy:
- Tumours: The most common reason for parotidectomy is the presence of a tumour in the parotid gland. Most parotid tumours are benign (non-cancerous), but some can be malignant (cancerous).
- Sialadenitis: Chronic inflammation of the parotid gland, causing pain and swelling, might necessitate parotidectomy in severe cases.
- Sialolithiasis: Salivary stones blocking the salivary ducts within the parotid gland can be treated with parotidectomy if other methods fail.
Types of Parotidectomy:
The type of parotidectomy performed depends on the location and size of the tumour or abnormality:
- Superficial Parotidectomy: Removes all or part of the superficial lobe of the parotid gland, located closer to the skin’s surface.
- Total Parotidectomy: Removes the entire parotid gland, including both superficial and deep lobes.
- Submandibular Parotidectomy: In rare cases, both the parotid gland and the submandibular gland (another salivary gland under the jaw) might be removed together.
Pre-Operative Evaluation:
Before surgery, various tests help determine the nature of the parotid gland issue and guide the surgical approach:
- Fine-needle aspiration (FNA): A thin needle is inserted into the parotid gland to collect a sample of cells for microscopic examination to differentiate between benign and malignant tumours.
- Imaging tests: CT scan or MRI scan provide detailed images of the parotid gland and surrounding structures to assess the tumor’s size, location, and potential involvement of facial nerves.
The Parotidectomy Procedure:
- Preparation: Performed under general anaesthesia in a hospital setting.
- Incision: The surgeon makes an incision in the crease in front of the ear, minimizing scarring.
- Facial Nerve Identification: Identifying and carefully dissecting the facial nerve, which runs through the parotid gland, is crucial to avoid facial paralysis as a complication.
- Gland Removal: Depending on the type of parotidectomy, all or part of the parotid gland is meticulously removed. In some cases, lymph nodes in the neck might also be removed for cancer staging.
- Wound Closure: The facial nerve is protected, and the surgical site is closed with stitches or surgical glue.
Facial Nerve Monitoring:
During surgery, special techniques like nerve monitoring are often used to continuously assess the health of the facial nerve, minimizing the risk of facial paralysis.
Potential Complications of Parotidectomy:
- Facial Paralysis: Damage to the facial nerve during surgery can lead to temporary or permanent weakness or paralysis of facial muscles on the affected side.
- Frey Syndrome: This condition causes sweating on the side of the face where the parotid gland was removed, particularly when eating or tasting.
- Bleeding: As with any surgery, there’s a risk of bleeding during or after surgery.
- Infection: Infection at the incision site is a potential complication.
- Numbness: Temporary numbness around the incision area can occur.
Recovery and Follow-Up:
- Hospital Stay: The length of stay depends on the type of surgery and potential complications. Typically, patients stay for 1-3 days for observation and pain management.
- Facial Exercises: Depending on the extent of facial nerve involvement, facial exercises might be recommended to help regain muscle function.
- Scar Care: Instructions are provided for incision care to minimize scarring.
- Follow-Up Appointments: Regular check-ups with the doctor are crucial to monitor the incision site, facial nerve function, and overall health.
- Cancer Treatment (if applicable): If the parotid tumour is malignant, additional cancer treatment like radiation therapy might be necessary.
Living After Parotidectomy:
- The recovery process varies depending on the type of surgery, presence of complications, and individual healing factors.
- Facial nerve function: Some patients may experience temporary facial weakness that gradually improves. In rare cases, permanent facial paralysis might occur.
- Return to normal activities: Most people can resume normal activities within a few weeks or a month after surgery, depending on the complexity of the procedure and recovery progress.
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.
SUBMANDIBULAR GLAND EXCISION
Submandibular Gland Excision: A Detailed Look at Removing the Submandibular Gland
The submandibular glands are one of the three pairs of major salivary glands in the mouth. Located under the jaw on either side of the tongue, these glands produce saliva, essential for digestion and maintaining oral health. Submandibular gland excision, also known as submandibular gland removal, is a surgical procedure to address problems within this gland.
Reasons for Submandibular Gland Excision:
There are several reasons why a doctor might recommend submandibular gland excision:
- Tumours: The most common reason for surgery is the presence of a tumour in the submandibular gland. These tumours can be benign (noncancerous) or malignant (cancerous). While most submandibular gland tumours are benign, surgery is often recommended for definitive diagnosis and removal to prevent potential complications.
- Sialolithiasis: This refers to a salivary stone (sialolith) blocking a salivary duct, causing pain, swelling, and difficulty opening the mouth. Depending on the stone’s location and size, surgery may be necessary for removal.
- Sialadenitis: This is an inflammation of the submandibular gland, which can be caused by infection, bacterial build-up, or autoimmune conditions. In cases where medication and conservative management fail, surgery may be considered to remove the affected gland.
- Chronic Sialadenitis: In some cases, recurrent or chronic inflammation can lead to damage and dysfunction of the gland, necessitating surgical removal.
Types of Submandibular Gland Excision:
The type of excision chosen depends on the specific reason for surgery and the size and location of the mass. Here are the main approaches:
- Total Submandibular Gland Excision: This involves removing the entire submandibular gland. It’s typically performed for large tumours or recurrent tumours.
- Superficial Submandibular Gland Excision: This removes only the superficial portion of the gland, leaving the deeper portion intact. This approach is preferred for smaller, benign lesions.
- Partial Submandibular Gland Excision: This removes a specific portion of the submandibular gland containing the tumour or sialolith. This approach aims to preserve as much healthy gland tissue as possible.
Pre-Operative Preparation:
Before surgery, a series of tests will be conducted to determine the nature of the problem and plan the appropriate surgical approach. This may include:
- Fine-Needle Aspiration (FNA): A thin needle is inserted into the mass to withdraw a small sample of cells for microscopic examination to differentiate between benign and malignant tumours.
- Imaging Studies: X-rays, CT scans, and MRIs can help determine the size, location, and extent of the mass and its relationship to surrounding structures.
- Sialography: In some cases, a special X-ray using contrast dye injected into the salivary duct system can help visualize any blockages or abnormalities.
Procedure:
A submandibular gland excision is typically performed under general anaesthesia. Here’s a breakdown of the steps for a total submandibular gland excision:
- Anaesthesia: You’ll receive general anaesthesia to ensure comfort and immobility during surgery.
- Incision: The surgeon makes an incision under the jaw, along the lower border of the mandible, typically on the side where the affected gland is located. This incision is designed to minimize scarring.
- Gland Dissection: The surgeon carefully dissects the submandibular gland from surrounding tissues, blood vessels, and nerves. The lingual nerve, which provides sensation to the tongue, is located near the gland, and meticulous dissection is crucial to avoid injuring it.
- Facial Nerve Considerations: While the facial nerve is not directly involved with the submandibular gland, its branches may be in close proximity. The surgeon takes precautions to avoid any inadvertent injury.
- Gland Removal: The entire submandibular gland is carefully removed.
- Closure: The surgical team closes the incision with sutures and applies a drainage tube to remove any excess fluid.
Recovery and Follow-Up:
- Hospital Stay: The length of stay depends on the type of surgery and potential complications. Typically, patients go home the same day or stay overnight for observation in minimally invasive cases.
- Pain Management: Pain medication is prescribed to manage post-surgical discomfort.
- Scar Care: Instructions are provided on caring for the incision to minimize scarring.
- Diet: Depending on the surgery’s extent, a soft diet might be recommended initially.
- Follow-Up Appointments: Regular check-ups with the doctor are crucial to monitor the incision site, overall healing, and address any lingering concerns.
- Cancer Treatment (if applicable): If the submandibular gland tumour is malignant, additional cancer treatment like radiation therapy might be necessary.
Living After Submandibular Gland Excision:
- Most patients experience significant improvement in symptoms like pain, swelling, or difficulty eating after successful surgery.
- Dry mouth management: Artificial saliva or other strategies might be recommended if persistent dryness becomes a concern.
- Return to normal activities: Most people can resume normal activities within a few days or a week after surgery, depending on the complexity of the procedure and recovery progress.
Additional Considerations:
- Minimally Invasive Techniques: In some cases, laparoscopic or robotic-assisted techniques
Disclaimer: This information is intended for general knowledge only and does not constitute medical advice. Please consult with your healthcare professional for diagnosis and treatment planning based on your specific situation.